
An Urban Institute
Program to Assess
Changing Social Policies
Health
Policy for
Low-Income
People in
Florida
Health
Policy for
Low-Income
People in
Florida
Debra J. Lipson
Stephen Norton
Lisa Dubay
The Urban Institute
State Reports
Assessing
the New
Federalism

An Urban Institute
Program to Assess
Changing Social Policies
Health
Policy for
Low-Income
People in
Florida
Debra J. Lipson
Stephen Norton
Lisa Dubay
The Urban Institute
Assessing
the New
Federalism
State Reports
The Urban
Institute
2100 M Street, N.W.
Washington, D.C. 20037
Phone: 202.833-7200
Fax: 202.429-0687
E-Mail: [email protected]
http://www.urban.org

Copyright q December 1997. The Urban Institute. All rights reserved. Except for short quotes, no part of this book may
be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, record-
ing, or by information storage or retrieval system, without written permission from The Urban Institute.
This report has been prepared as part of The Urban Institute’s Assessing the New Federalism project, which has
received funding from the Annie E. Casey Foundation, the Henry J. Kaiser Family Foundation, the W.K. Kellogg
Foundation, the John D. and Catherine T. MacArthur Foundation, the Commonwealth Fund, the Robert Wood Johnson
Foundation, the McKnight Foundation, and the Fund for New Jersey. Additional funding is provided by the Joyce
Foundation and the Lynde and Harry Bradley Foundation through a subcontract with the University of Wisconsin at
Madison.
The views expressed are those of the authors and should not be attributed to The Urban Institute or its funders.
The authors thank the many state, county, and local officials and others who participated in interviews and pro-
vided information.
About the Series
A
ssessing the New Federalism is a multi-year Urban Institute project
designed to analyze the devolution of responsibility from the federal
government to the states for health care, income security, employ-
ment and training programs, and social services. Researchers monitor
program changes and fiscal developments, along with changes in family well-
being. The project aims to provide timely nonpartisan information to inform
public debate and to help state and local decisionmakers carry out their new
responsibilities more effectively.
Key components of the project include a household survey, studies of poli-
cies in 13 states, and a database with information on all states and the District
of Columbia, available at the Urban Institute’s Web site. This paper is one in a
series of reports on the case studies conducted in the 13 states, home to half of
the nation’s population. The 13 states are Alabama, California, Colorado,
Florida, Massachusetts, Michigan, Minnesota, Mississippi, New Jersey, New
York, Texas, Washington, and Wisconsin. Two case studies were conducted in
each state, one focusing on income support and social services, including
employment and training programs, and the other on health programs. These 26
reports describe the policies and programs in place in the base year of this pro-
ject, 1996. A second set of case studies to be prepared in 1998 or 1999 will
describe how states reshape programs and policies in response to increased
freedom to design social welfare and health programs to fit the needs of their
low-income populations.
The income support and social services studies look at three broad areas.
Basic income support for low-income families, which includes cash and near-
cash programs such as Aid to Families with Dependent Children and Food
Stamps, is one. The second area includes programs designed to lessen the

dependence of families on government-funded income support, such as educa-
tion and training programs, child care, and child support enforcement. Finally,
the reports describe what might be called the last-resort safety net, which
includes child welfare, homeless programs, and other emergency services.
The health reports describe the entire context of health care provision for
the low-income population. They cover Medicaid and similar programs, state
policies regarding insurance, and the role of public hospitals and public health
programs.
In a study of the effects of shifting responsibilities from the federal to state
governments, one must start with an understanding of where states stand.
States have made highly varied decisions about how to structure their
programs. In addition, each state is working within its own context of private-
sector choices and political attitudes toward the role of government. Future
components of Assessing the New Federalism will include studies of the varia-
tion in policy choices made by different states.
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
iv

Contents
Highlights of the Report 1
Overview of Florida 5
Sociodemographic 5
Economic 5
Political 6
Roadmap to the Rest of the Report 8
Setting the Policy Context 9
Overview of the State’s Health Care Agenda 9
State Health and Health Care Indicators 11
Health Care Spending and Coverage 11
Organizational Structure of State Health Programs 17
Assessing the New Federalism: Potential State Responses to Additional
Flexibility and Reduced Funding 19
General State Philosophy toward the Poor 19
Medicaid-Specific Issues 20
Providing Health Coverage for Low-Income People 21
Medicaid Eligibility 21
Other Public Financing Programs 24
Insurance Reforms 25
Financing and Delivery System 27
Commercial Managed Care 27
Hospital Market and Regulatory Issues 29
Mergers and For-Profit Conversions 29
Medicaid Provider Reimbursement (including DSH Payments) 30
Medicaid Managed Care 32

Delivering Health Care to the Uninsured Population 37
State and County Public Health Programs 37
Impact of Government Policies and Market Changes on Safety Net
Providers in Dade and Hillsborough Counties 38
Long-Term Care for the Elderly and Persons with Disabilities 45
Supply, Expenditures, and Utilization 45
Long-Term Care for the Elderly 47
Younger People with Disabilities 50
Challenges for the Future 53
Notes 57
Appendix: List of People Interviewed 61
About the Authors 65
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
vi
Highlights of the Report
H
ealth policy issues have been a priority for Florida under the leader-
ship of Governor Lawton Chiles. The Florida Health Security Plan,
which Governor Chiles proposed in 1992 and which was ultimately
rejected by the state legislature, represented an expansion of insur-
ance coverage together with a managed competition approach to controlling
health costs. Governor Chiles was successful in winning passage of insurance
reforms in the private insurance market. In 1997, the governor made expan-
sion of coverage to children through Medicaid and the state’s Healthy Kids
Program his top health priority. He also brought suit against the U.S. govern-
ment to seek relief from changes in welfare laws that affected many legal non-
citizens in Florida and opposed the formula for distributing federal block grant
funds in 1995 because of its likely negative impact on the state of Florida.
Florida has a number of health care problems. It has one of the highest un-
insured rates in the country, 19.2 percent (vs. 15.5 percent for the nation). Per
capita spending on Medicaid ranks as one of the lowest in the country (46th
nationally) despite having the fourth largest Medicaid enrollment, about 2.2
million. The state ranks near the bottom (i.e., worst) on a number of measures of
health status, including the number of premature deaths per capita, prevalence
of cancer, number of AIDS cases, and rate of violent crime.
Medicaid enrollment and expenditure growth accelerated in the 1990s.
Between 1990 and 1995, enrollment grew by 12.7 percent annually, expendi-
tures, by 18.7 percent. Spending grew by 27.2 percent between 1990 and 1992,
and by 13.4 percent per year between 1992 and 1995. Florida’s eligibility stan-
dards remain low by national standards. In 1994, 39.6 percent of the low-
income population below 150 percent of the federal poverty level (FPL) had
Medicaid coverage compared with 51 percent nationally. The state has a some-

what restrictive benefit package and spends less per enrollee than the national
average for all eligibility groups except children. Expenditures on long-term
care are low despite a large elderly population. The number of nursing home
beds per elderly person is well below the national average, and there is minimal
coverage of home and community-based services.
Managed care is the cornerstone of the state’s efforts to control Medicaid
acute care expenditures. Florida now contracts with 19 health maintenance
organizations (HMOs) and has implemented a primary care case management
program (MediPass) throughout the state. The state now requires mandatory
enrollment in managed care for most recipients—two-thirds of Medicaid bene-
ficiaries are in either MediPass or capitated managed care plans. Florida has
had a history of marketing and enrollment abuses and problems with quality
of care in managed care programs. Recently, the state prohibited direct market-
ing, increased resources for beneficiary education, and added staff to monitor
quality of care. It has also enacted a competitive bidding system to drive down
capitation rates, hoping to reduce rates to 92 percent of fee-for-service rates.
The state also faces problems resulting from the impact of recent welfare
reform legislation on future legal immigrants. At the time of the site visit, it was
estimated that 54,000 current Supplemental Security Income (SSI) recipients in
Florida would lose their SSI and Medicaid benefits, and another 3,062 immi-
grants who were receiving Medicaid were also expected to lose coverage. The
state filed suit asking the federal court to declare that denying SSI and food
stamp benefits to otherwise eligible, lawful, permanent resident aliens is uncon-
stitutional. Legislation was introduced by the Dade County delegation to main-
tain coverage for these individuals at state or local expense. The cost to the state
(or to local areas) was estimated at $222 million. While the Balanced Budget
Act of 1997 ensures that most of these individuals will retain their benefits,
future immigrants will not be covered.
To reduce the number of uninsured children, the governor has proposed
expanding Medicaid to cover children ages 0 to 3 old years in households with
income up to 185 percent of the FPL. The state is also expanding its Healthy
Kids Program. The Healthy Kids Program is a school enrollment–based insur-
ance program that currently provides comprehensive health insurance coverage
to 26,400 children. Additional funding has been granted to increase the number
of children in the program to 60,000. The legislature recently granted the
Agency for Health Care Administration the authority to seek a Section 1115
waiver to cover children in households with income up to 185 percent of the
FPL through the Healthy Kids Program. The cost of the program averages about
$600 per child. The program is able to keep the costs below Medicaid because
of limits on the number of plans, because of some restrictions on benefits, and
because the population served is relatively healthy.
Florida has enacted a series of insurance reforms. The reforms require insur-
ers offering policies in the small-group market to guarantee issue of policies
without regard for health status or preexisting conditions, provide for portabil-
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
2

ity of plans between employers, and require the use of modified community rat-
ing. The legislation does not affect the individual insurance market. Florida
also created 11 regional Community Health Purchasing Alliances (CHPAs) in an
attempt to reduce the costs of health insurance in the small-group market.
Currently 18,000 small businesses representing 76,000 individuals receive
coverage through the CHPAs. It appears the state is experiencing a certain
amount of adverse selection in the CHPAs. The CHPAs are also prohibited from
negotiating rates with insurers, limiting their ability to take advantage of their
market power. As a result, premiums for CHPA-sponsored insurance plans are
reportedly only about 6 percent less than premiums for the same plans offered
outside of the CHPAs.
Managed care has been growing rapidly in the private market in Florida.
As of 1995, 25 percent of the state’s population was enrolled in an HMO. Much
of the growth has been among for-profit HMOs. Although the largest HMOs
remain profitable, many of the smaller HMOs have experienced losses. As a
result, mergers and acquisitions are now occurring frequently in the commer-
cial HMO market. State policy has generally been supportive of the growth of
managed care. A number of bills to regulate managed care have been introduced
in the legislature, but to date few have been enacted. The 1997 legislative ses-
sion is expected to include increased efforts to enact legislation to set standards
for HMO practices.
The hospital market has a considerable amount of excess capacity. As a
result, HMOs and other managed care plans have successfully negotiated deep
discounts. There has also been considerable growth in for-profit hospital sys-
tems, although some nonprofit hospital systems are also developing rapidly.
However, to date there has been little impact on the number of hospitals and
number of beds. While there is concern over the implications of the growing
number of for-profit hospital beds on the provision of charity care, no action has
been taken. In fact, Columbia/HCA and the South Florida Hospital Association
have challenged the tax-exempt status of nonprofit hospitals, arguing that many
nonprofits provide little charity care but still receive tax benefits not available
to for-profit hospitals.
Safety net hospitals face significant competitive pressures as the growth in
Medicaid managed care increases the interest of private hospitals in the
Medicaid market. Nonetheless, they appear to be doing reasonably well in gen-
eral. One reason is an increase in local funding for indigent care. In both Dade
and Hillsborough Counties, local funding for indigent care has risen consider-
ably as a result of increases in sales taxes. In addition, hospitals are either devel-
oping their own HMOs or prepaid health plans, joining with other HMOs or
prepaid health plans, or developing networks with other health care providers
to achieve greater efficiencies.
Although the infusion of funds and their continuance are important to the
safety net’s success, the manner in which the funds are distributed is also
important. Hillsborough County has used the new tax revenues to fund an
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
THE URBAN
INSTITUTE
3

insurance program that distributes funds across several types of providers.
Nonetheless, Tampa General Hospital, the major public hospital, is losing its
Medicaid patient base and is increasingly reliant on state financial support.
Dade County’s new revenues are largely targeted to Jackson Memorial Hospital,
the county’s major public hospital. These revenues are permitting the hospital
to survive the loss of Medicaid revenues. Community clinics did not receive
any of these new funds and are facing serious problems. The big question is
whether local revenues will remain adequate and continue to support care for
the indigent in these counties, as well as in other sites throughout the state.
Despite its large elderly population, Florida has relatively low expenditures
on long-term care. Long-term care is 28 percent of the state’s Medicaid budget,
compared with the national average of 34 percent. Long-term care spending is
low in Florida because its nursing home bed supply (30 beds per 1,000 people
over age 65) is one of the lowest in the country and because it has been slow to
expand home and community-based services. The state now has a few home
and community-based waiver programs and is experimenting with increases
in the provision of these services. Increases in expenditures for long-term care
seem inevitable but could place added pressures on Medicaid spending for
other groups.
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
4
Overview of Florida
Sociodemographic
F
lorida has one of the country’s biggest and most diverse state popula-
tions. In 1995, Florida had a population of 14.1 million, which had
increased 9.5 percent since 1990, or 1.7 times faster than the growth rate
of the U.S. population (table 1). One in six people (16.2 percent) in the
state had income below the federal poverty level (FPL) in 1994, compared with
about one in seven people (14.3 percent) nationwide. Compared with the
United States as a whole, Florida has a higher proportion of Hispanics (16.5
percent vs. 10.7 percent in 1995). The Miami area is notable for its large con-
centration of Cubans. Overall, 10.0 percent of the state’s population in 1995
were immigrants, compared with 6.4 percent for the nation.
In 1995, 2.7 million people, or 16.7 percent of the state’s population, were
over the age of 65, substantially higher than the national average of 12.1 percent
and higher than in any other state. Its elderly population is also one of the
fastest growing in the country; the state projects a 35 percent growth in the
age-80-and-older population in the next 10 years. The majority of the state’s
population resides in a half dozen major urban centers (e.g., Miami/Fort
Lauderdale, Tampa/St. Petersburg, Orlando, and Jacksonville). Although the
state has large rural areas, there are very few places located more than an hour
from a medium-sized city.
Economic
Florida’s economy is healthy and growing at a faster rate than the U.S. econ-
omy as a whole. Job growth during FY 97–98 is projected to be 2.9 percent,
more than double the U.S. rate of 1.3 percent.
1
Beyond that, Florida’s state bud-
get assumes a slight deceleration of output and spending, which will result in
somewhat slower growth in its economy. The unemployment rate was slightly
less than that for the United States as a whole in 1996 (5.1 percent versus 5.4
percent). Per capita income ($23,061) is about on a par with the national aver-
age ($23,208) as was the increase in per capita income from 1990 to 1995—
20.7 percent in the state versus 21.2 percent in the nation (table 1). In part
because of the strong economy, Aid to Families with Dependent Children
(AFDC) caseloads have declined in each of the last three fiscal years, dropping
from about 220,500 families in October 1995 to 186,600 families in December
1996. These declines have continued since the implementation of the state’s
welfare reform program.
Political
Governor Lawton Chiles, a Democrat, has been in office since 1991 and won
reelection in 1994; his current term expires in 1998, and Florida law prohibits
him from running for a third consecutive term. Florida’s legislature has histor-
ically been led by Democrats, but that has changed recently. The Florida Senate
was evenly split prior to the 1994 election, when Republicans gained a majority
of the seats. In 1996, Republicans also gained majority control of the House,
with a two-seat lead (61 to 59). Republicans retained control over the Senate
in 1996 and now have a six-seat margin over Democrats (23 to 17).
Between 1994 and 1996, Governor Chiles’s relations with the split-control
legislature were marked by some tension. While there has been bipartisan sup-
port for spending on corrections and education throughout the 1990s, the leg-
islature has recently opposed some of the governor’s health initiatives. The
legislative agenda was dominated by a debate over funding priorities, cast
largely as a trade-off between social and health services versus education and
corrections. The legislature took funds proposed for Medicaid and transferred
them to corrections and education. With a change in legislative leadership and
a takeover of the House by Republicans, it was a matter of some speculation
whether the governor would be able to have any of his health initiatives
approved.
Health policy issues have been a particularly high priority of the gover-
nor. He sought passage of two pieces of legislation (the Health Care Reform Act
of 1992 [Chapter 92-33] and the Health Care and Insurance Reform Act of 1993
[Ch. 93-129]), which together promised to ensure for all Floridians “access to
a basic health care benefit package . . . by December 31, 1994.” The Health Care
Reform Act of 1992 created the Agency for Health Care Administration
(AHCA) to help ensure that that goal was reached. The Health Care and
Insurance Reform Act of 1993 provided the authority to create Community
Health Purchasing Alliances (CHPAs), fund rural health network initiatives,
and seek federal waivers to expand Medicaid eligibility to those with incomes
up to 250 percent of the FPL. Both acts included insurance market reforms.
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
6
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
THE URBAN
INSTITUTE
7
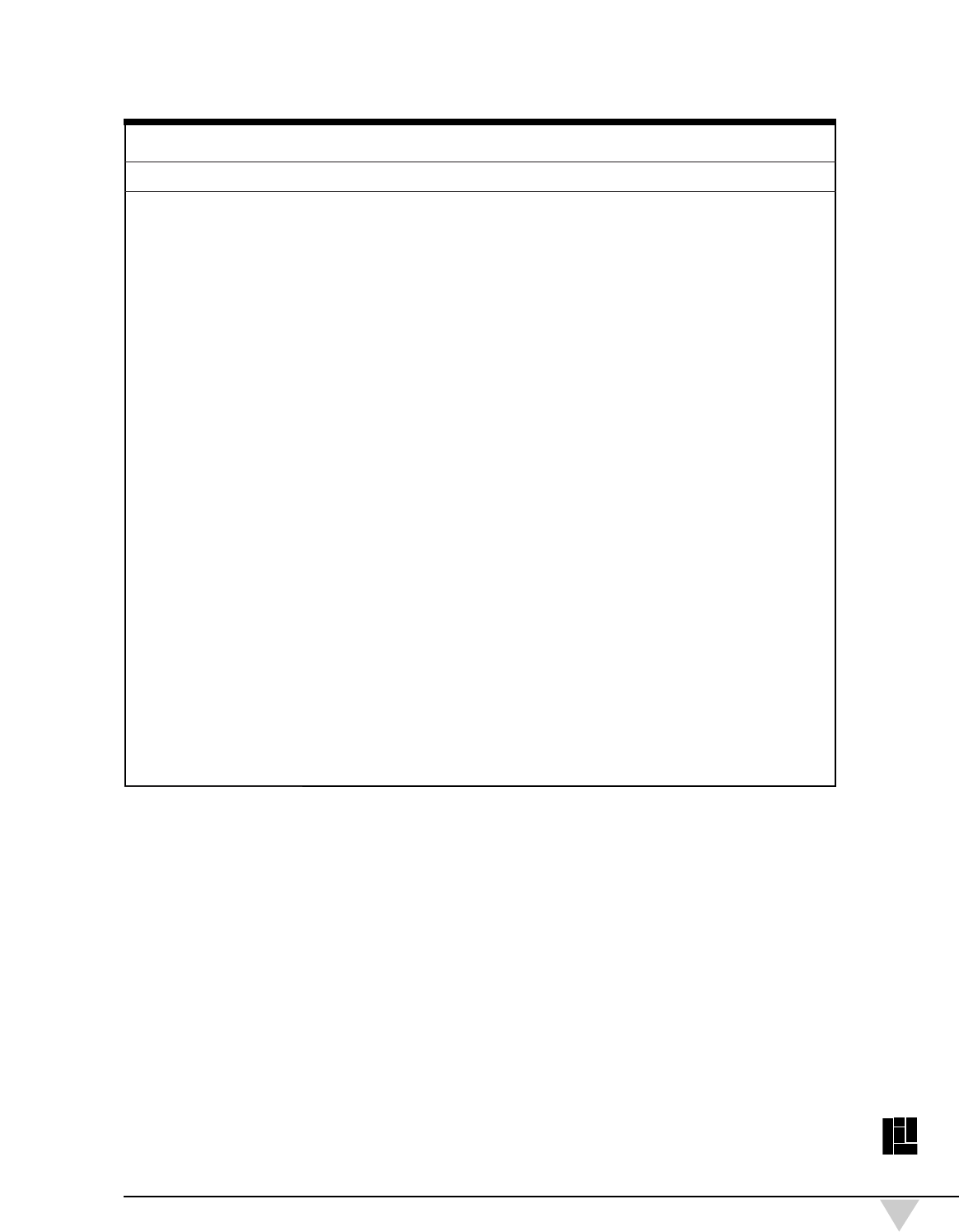
Table 1State Characteristics
Florida United States
Sociodemographic
Population (1994–95)
a
(in thousands) 14,103 260,202
Percent under 18 (1994–95)
a
24.6% 26.8%
Percent 65+ (1994–95)
a
16.7% 12.1%
Percent Hispanic (1994–95)
a
16.5% 10.7%
Percent Non-Hispanic Black (1994–95)
a
15.4% 12.5%
Percent Non-Hispanic White (1994–95)
a
66.5% 72.6%
Percent Non-Hispanic Other (1994–95)
a
1.6% 4.2%
Percent Noncitizen Immigrant (1996) * 10.0% 6.4%
Percent Nonmetropolitan (1994–95)
a
6.9% 21.8%
Population Growth (1990-95)
b
9.5% 5.6%
Economic
Per Capita Income (1995)
c
$23,061 $23,208
Percent Change in Per Capita Personal Income (1990–95)
c, d
20.7% 21.2%
Percent Change in Personal Income (1990–95)
c, e
31.3% 27.7%
Employment Rate (1996)
f, g
58.8% 63.2%
Unemployment Rate (1996)
f
5.1% 5.4%
Percent below Poverty (1994)
h
16.2% 14.3%
Percent Children below Poverty (1994)
h
25.9% 21.7%
Health
Percent Uninsured—Nonelderly (1994–95)
a
19.2% 15.5%
Percent Medicaid—Nonelderly (1994–95)
a
13.2% 12.2%
Percent Employer Sponsored—Nonelderly (1994–95)
a
59.2% 66.1%
Percent Other Health Insurance—Nonelderly (1994–95)
a, i
8.5% 6.2%
Smokers among Adult Population (1993)
j
22.0% 22.5%
Low Birth-Weight Births (<2,500 g) (1994)
k
7.7% 7.3%
Infant Mortality Rate (Deaths per 1,000 Live Births) (1995)
l
7.5 7.6
Premature Death Rate (Years Lost per 1,000) (1993)
m, n
59.6 54.4
Violent Crimes per 100,000 (1995)
o
1,071.0 684.6
AIDS Cases Reported per 100,000 (1995)
j
56.9 27.8
Political
Governor’s Affiliation (1996)
p
D
Party Control of Senate (Upper) (1996)
p
17D-23R
Party Control of House (Lower) (1996)
p
59D-61R
a. Two-year concatenated March Current Population Survey (CPS) files, 1995 and 1996. These files are edited by the Urban
Institute’s TRIM2 microsimulation model. Excludes those in families with active military members.
b. U.S. Bureau of the Census, Statistical Abstract of the United States: 1996(116th edition). Washington, D.C., 1996. 1995 popu-
lation as of July 1. 1990 population as of April 1.
c. State Personal Income, 1969-1995.CD-ROM. Washington, D.C.: Regional Economic Measurement Division (BE-55), Bureau of
Economic Analysis, Economics and Statistics Administration, U.S. Department of Commerce, October 1996.
d. Computed using mid-year population estimates of the Bureau of the Census.
e. Personal contributions for social insurance are not included in personal income.
f. U.S. Department of Labor. State and Regional Unemployment, 1996 Annual Averages.USDL 97-88. Washington, D.C., March
18, 1997.
g. Employment rate is calculated using the civilian noninstitutional population 16 years of age and over.
h. CPS three-year average (March 1994–March 1996 where 1994 is the center year) edited using the Urban Institute’s TRIM2
microsimulation model.
i. “Other” includes persons covered under CHAMPUS, VA, Medicare, military health programs, and privately purchased
coverage.
j. Normandy Brangen, Danielle Holahan, Amanda H. McCloskey, and Evelyn Yee. Reforming the Health Care System: State
Profiles 1996.Washington, D.C.: American Association of Retired Persons, 1996.
k. S.J. Ventura, J.A. Martin, T.J. Mathews, and S.C. Clarke. “Advance Report of Final Natality Statistics, 1994.” Monthly Vital
Statistics Report; vol. 44, no. 11, supp. Hyattsville, MD: National Center for Health Statistics, 1996.
l. National Center for Health Statistics. “Births, Marriages, Divorces, and Deaths for 1995.” Monthly Vital Statistics Report; vol.
44, no. 12. Hyattsville, MD: Public Health Service, 1996.
m. ReliaStar Financial Corporation. The ReliaStar State Health Rankings: An Analysis of the Relative Healthiness of the
Populations in All 50 States, 1996 edition, Minneapolis, MN:ReliaStar, 1996.
n. Race-adjusted data, National Center for Health Statistics, 1993 data.
o. U.S. Department of Justice, FBI. Crime in the United States, 1995.October 13, 1996.
p. National Conference of State Legislatures. 1997 Partisan Composition, May 7 Update.D indicates Democrat and R indicates
Republican.

The CHPAs were established in 1994, a number of rural health networks have
been certified by AHCA, and there has been significant reform in the small-
group insurance market. However, the Florida Health Security Act, the state’s
Section 1115 waiver that emerged from the 1993 act, never received funding
from the legislature.
The governor, although an ally of the Clinton administration, has not hesi-
tated to challenge federal policies that adversely affect Florida. For example,
in April 1997 he filed suit against the U.S. government, seeking relief from
changes in federal welfare laws that restrict essential federal benefits for many
legal noncitizens in Florida. He was a supporter of federal welfare reform, but
he expressed great concern about the spending caps in the 1995 Medicaid block
grant proposal. He believed the caps would be unfair to Florida and other high
population-growth states or those that had low per capita expenditures, because
those states would have a harder time finding savings.
Although it is often thought that Cubans and other Latin Americans consti-
tute the largest source of immigrants to the state, “immigrants from the North”
(the snowbelt states) constitute a much larger proportion of the state’s growing
population. Nonetheless, the delegates from the Miami area are considered a
powerful group in the legislature.
About 72 percent of the state’s general revenue ($15.6 billion in FY 96–97)
comes from sales tax collections.
2
The state does not have an income tax, and
only counties can impose ad valorem (property) taxes. For FY 97–98, the
Florida Consensus Estimating Conference projects the state’s general revenue
growth at 4.7 percent, or $757 million more in recurring general revenue, and
projects an overall revenue growth of 5 percent. This is down, however, from
the average annual rate of 8 percent in the last 10 years, when the introduction
of the Florida lottery and an infusion of federal funds because of rising
Medicaid and AFDC caseloads contributed to a higher growth rate.
Roadmap to the Rest of the Report
The remainder of this report lays out the major issues, initiatives, and chal-
lenges in health care facing the state policymakers in the spring of 1997. It
describes the state’s current health care agenda and recent spending trends,
describes the organizational structure of state health programs, and gives some
sense of prevailing state and local attitudes toward meeting the health care
needs of the poor. It then delves into the details of Medicaid eligibility, man-
aged care programs, provider reimbursement, and long-term care policy. The
report describes how state policies are affecting the health care delivery sys-
tem for poor people in two communities—Dade County, home to Miami, and
Hillsborough County, which includes Tampa. It concludes with a discussion
of the major challenges facing the state.
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
8
Setting the Policy Context
Overview of the State’s Health Care Agenda
T
hree significant health care issues consumed the attention of state offi-
cials and advocates at the time of the site visit: (1) awards of new
Medicaid capitated managed care contracts and attempts to shift
MediPass program participants into capitated plans; (2) a number of
children’s health initiatives, including an expansion of the Healthy Kids
Program, which subsidizes insurance premiums for low-income, school-aged
children, and expansion of Medicaid eligibility to children ages 1 through 3 in
families earning up to 185 percent of the FPL; and (3) concerns about the impact
of federal welfare reform and immigration laws on Medicaid eligibility for legal
immigrants.
Florida’s Medicaid managed care program experienced significant problems
two years ago when contracting plans’ marketing abuses, quality of care prob-
lems, and charges of excess profit-taking were the focus of a series of articles
in the Fort Lauderdale Sun Sentinel. The publicity led to several legislative
changes in 1995, including prohibitions on direct marketing, rate rollbacks of
between 8 and 18 percent, and the addition of Medicaid staff to monitor health
plans’ quality of care. In 1996, the legislature mandated assignment into either
MediPass, the primary care case management program, or a health maintenance
organization (HMO) or prepaid health plan (PHP) (previously recipients were
required to enroll only in MediPass). The legislature also mandated a competi-
tive bidding process for HMOs, setting a maximum capitation rate of 92 percent
of fee-for-service (FFS) rates, and it authorized more enrollee education regard-
ing managed care choices. Both the administration and the legislature have

focused on implementing these changes, addressing, in particular, problems
with the schedule and outcome of the bidding process.
In his FY 97–98 budget, the governor’s biggest priority was a set of chil-
dren’s initiatives that included 22 separate programs.
3
The most important was
the expansion of the Healthy Kids Program and Medicaid for young children,
consistent with the governor’s previous attempts to expand insurance coverage.
Despite his focus on children, who generally garner more support across the
aisle, the governor faced some roadblocks. Republican leaders in the legislature
expressed their strong opposition to creating any new “middle-class entitle-
ments,” and they seemed more interested in further Medicaid budget cuts than
in anything that would increase Medicaid spending.
Federal welfare reform legislation (the Personal Responsibility and Work
Opportunity Reconciliation Act of 1996—PRWORA) restricted immigrants’
eligibility for a wide range of benefits, including Medicaid. Prior to welfare
reform, legal noncitizens were eligible for Medicaid on the same basis as citi-
zens. The new law bars immigrants arriving after passage of the law (August 22,
1996) from receiving Medicaid for their first five years in the country. It also
gives states the option of providing Medicaid to immigrants already in the
United States.
At the time of the site visit, the state had made clear its intent to continue
Medicaid coverage for legal immigrants residing in the state who qualify for
Supplemental Security Income (SSI) or AFDC/Temporary Assistance to Needy
Families (TANF) or who meet other Medicaid eligibility requirements.
Nonetheless, the state estimated that about 3,062 current Medicaid recipients
(not including SSI recipients) would likely be ineligible for Medicaid (66 per-
cent of whom reside in Dade County) under the federal welfare reform law, even
after accounting for those who would remain eligible because of exceptions,
naturalization, or state options. About 54,000 people would have lost SSI ben-
efits, with approximately 74 percent living in Dade County.
4
However, the pas-
sage of the Balanced Budget Act of 1997 grandfathered SSI recipients present in
the United States as of August 22, 1996. As a result, most of the estimated
54,000 will not lose their benefits. Nonetheless, future immigrants will not be
covered by Medicaid for their first five years in the country, which will put pres-
sure on the state and local areas.
Observers were very concerned that many of those people who would have
lost coverage under the old rules would end up in nursing homes because they
could not afford rent or food to stay in the community. A legislative staffer
estimated that changes in Medicaid rules for legal immigrants before the enact-
ment of the Balanced Budget Act would have cost the state around $243 mil-
lion; if a quarter of the people losing SSI coverage moved into a nursing home,
state expenditures could have increased by about $432 million. Some believed
Miami nursing home representatives would successfully lobby the legislature
for such funds; others said it would depend on the state budget situation and
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
10
the way in which the media covered the issue. Similar uncertainties regarding
coverage of immigrants can be expected in the future under the new rules.
State Health and Health Care Indicators
Florida’s nonelderly uninsured rate of 19.2 percent is among the highest
state rates in the nation, exceeding the national average of 15.5 percent (table 1).
This may be attributable to the state’s service-dominated and small employer–
based economy. The rate has not decreased very much in the last few years,
despite the state’s overall strong economy. According to one source, Florida
ranks 38th lowest out of the 50 states with respect to an aggregation of health
indicators. Florida performs poorly on a number of health status measures: It
ranks in the bottom fifth of the country in the prevalence of infectious diseases,
motor vehicle deaths, and premature death rate and is ranked lowest (i.e.,
worst) with respect to the prevalence of cancer. The state has twice the rate of
AIDS cases as the national average and a 56 percent higher rate of violent crime.
Florida is closer to the U.S. average for such measures as low-birth-weight
births, infant mortality rates, and smoking among the adult population.
Health Care Spending and Coverage
Between FY 90–91 and FY 96–97, total average monthly caseloads under
the Medicaid program grew from 992,038 to 1,526,823—a 54 percent increase.
5
Most of the growth, however, occurred between FY 90–91 and FY 92–93,
because of recession-induced increases in AFDC caseloads and large increases
in the expanded eligibility groups—for instance, AFDC-Unemployed Parent
(UP), the medically needy program, poverty-related pregnant women and
infants (with income up to 185 percent of the FPL) and children, optional cov-
erage of elderly and disabled populations, and qualified Medicare beneficiaries.
Despite its eligibility expansions, Florida’s Medicaid program is still in the
bottom 10 states in percent of total low-income population covered.
The state has restricted benefits in order to limit acute and long-term care
costs; inpatient days are limited to 45, except for children, and the state does
not cover nursing home services for the medically needy. The state also does
not cover five optional services for the medically needy that it does cover for the
categorically needy: inpatient hospital services for persons over age 65 in insti-
tutions for mental disease, Intermediate Care Facility for the Developmentally
Disabled (ICF/DD) services, nursing facility services for individuals under age
21, case management services, and tuberculosis-related health services.
Florida’s Medicaid spending has increased as a share of all state expendi-
tures throughout the 1990s. Out of a total state 1995 budget of approximately
$35.9 billion, Medicaid’s share was $5.9 billion, or 16.5 percent, an increase
from 10.7 percent in 1990 (table 2). Medicaid’s share of state spending (exclud-
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
THE URBAN
INSTITUTE
11
ing federal funds) also increased over this same period, from $812 million
(7.0 percent of state-only spending) to $1.9 billion (13.1 percent of state-only
spending). During the same period, state expenditures on elementary and sec-
ondary education and higher education fell as a share of all state expenditures.
Medicaid annual growth rates declined from over 20 percent in the late
1980s and early 1990s to an estimated 3.8 percent between FY 94–95 and FY
95–96, “due in large part to the economic recovery.”
6
During the next four years,
the average growth per year was estimated by administration officials to be
about 6.7 percent.
In 1995, state general revenues made up 70.5 percent of the nonfederal
share of Medicaid expenditures; the remainder came from a variety of sources,
primarily the Public Medical Assistance Trust Fund (PMATF) (17 percent of
the nonfederal share).
7
The PMATF was created in 1984 to provide an ongoing
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
12
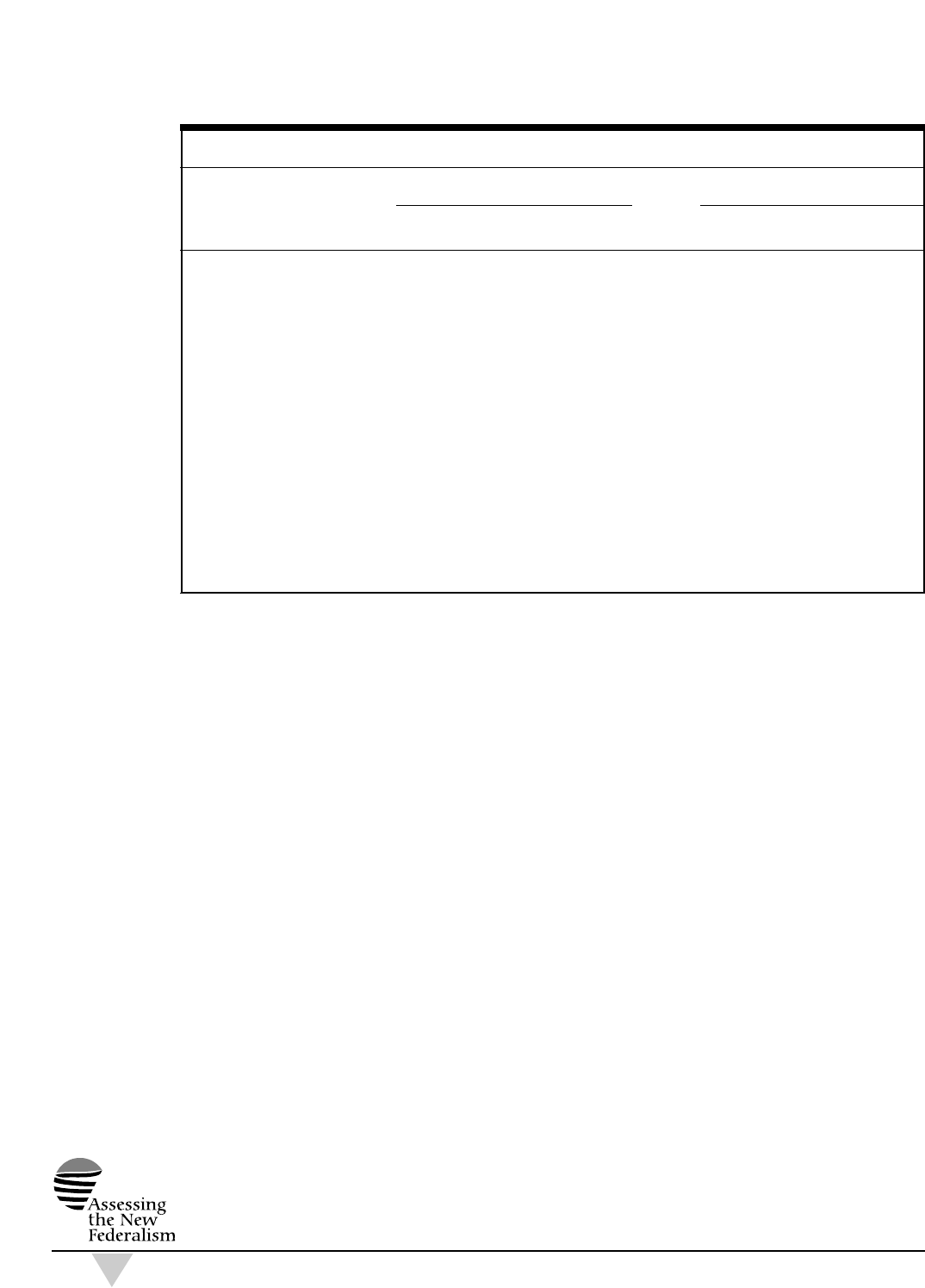
Table 2 Florida Spending by Category, 1990 and 1995 ($ in Millions)
State General-Fund Expenditures
a
Expenditures
b
Annual Annual
Program 1990 1995 Growth 1990 1995 Growth
Total $11,619 $14,649 4.7% $22,481 $35,907 9.8%
Medicaid
c, d
812 1,921 18.8 2,407 5,931 19.8
% of Total (7.0 ) (13.1 ) — (10.7 ) (16.5 ) —
Corrections 709 1,398 14.5 864 1,472 11.2
% of Total (6.1 ) (9.5 ) — (3.8 ) (4.1 ) —
K–12 Education 5,808 5,907 0.3 6,431 6,715 0.9
% of Total (50.0 ) (40.3 ) — (28.6 ) (18.7 ) —
AFDC 162 312 14.0 403 782 14.2
% of Total (1.4 ) (2.1 ) — (1.8 ) (2.2 ) —
Higher Education 1,536 1,663 1.6 2,321 1,999 (2.9)
% of Total (13.2 ) (11.4 ) — (10.3 ) (5.6 ) —
Miscellaneous
e
2,592 3,448 5.9 10,055 19,008 13.6
% of Total (22.3 ) (23.5 ) — (44.7 ) (52.9 ) —
Source: National Association of State Budget Officers, 1992 State Expenditure Report (April 1993) and 1996 State Expenditure
Report (April 1997).
a. State spending refers to general-fund expenditures plus other state fund spending for K–12 education.
b. Total spending for each category includes the general fund, other state funds, and federal aid.
c. States are requested by the National Association of State Budget Officers (NASBO) to exclude provider taxes, donations, fees, and
assessments from state spending. NASBO asks states to report these separately as “other state funds.” In some cases, however, a
portion of these taxes, fees, etc., is included in state spending because states cannot separate them. Florida reported other state funds
of $237 million in 1990 and $659 million in 1995.
d. Total Medicaid spending will differ from data reported on the HCFA 64 for three reasons: first, NASBO reports on the state fis-
cal year and the HCFA 64 on the federal fiscal year; second, states often report some expenditures, (e.g. mental health and/or mental
retardation) as “other health” rather than Medicaid; third, local contributions to Medicaid are not included, but would be part of
Medicaid spending on the HCFA 64.
e. This category includes all remaining state expenditures (e.g., environmental projects, transportation, housing, and other cash-
assistance programs) not captured in the five listed categories.
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
THE URBAN
INSTITUTE
13
Table 3 Medicaid Expenditures by Eligibility Group and Type of Service, Florida and United States (Expenditures in Millions)
Florida United States
Average Annual Average Annual
Expenditures Growth Expenditures Growth
1990 1992 1995 1990–92 1992–95 1990 1992 1995 1990–92 1992–95
Total $2,657.4 $4,298.1 $6,274.7 27.2% 13.4% $73,662.2 $118,926.0 $157,872.5 27.1% 9.9%
Benefits
Benefits by Service $2,490.5 $3,958.1 $5,799.9 26.1% 13.6% $69,168.7 $97,602.4 $133,434.6 18.8% 11.0%
Acute Care 1,626.2 2,784.7 4,030.7 30.9% 13.1% 36,904.5 55,059.9 79,438.5 22.1% 13.0%
Long-Term Care 864.4 1,173.4 1,769.3 16.5% 14.7% 32,264.2 42,542.5 53,996.1 14.8% 8.3%
Benefits by Group $2,490.5 $3,958.1 $5,799.9 26.1% 13.6% $69,168.7 $97,602.4 $133,434.6 18.8% 11.0%
Elderly $887.0 $1,229.4 $1,755.0 17.7% 12.6% $23,334.3 $31,757.9 $40,087.4 16.7% 8.1%
Acute Care 307.8 432.5 637.5 18.5% 13.8% 4,925.4 6,911.5 9,673.7 18.5% 11.9%
Long-Term Care 579.2 796.9 1,117.5 17.3% 11.9% 18,408.9 24,846.4 30,413.7 16.2% 7.0%
Blind & Disabled $779.3 $1,272.4 $1,908.6 27.8% 14.5% $25,771.6 $35,684.6 $51,379.4 17.7% 12.9%
Acute Care 497.1 908.7 1,276.1 35.2% 12.0% 12,929.2 19,483.6 29,760.7 22.8% 15.2%
Long-Term Care 282.2 363.8 632.5 13.5% 20.3% 12,842.4 16,201.0 21,618.7 12.3% 10.1%
Adults $370.3 $436.5 $505.9 8.6% 5.0% $8,765.0 $12,710.1 $16,556.9 20.4% 9.2%
Children $453.9 $1,019.8 $1,630.5 49.9% 16.9% $11,297.8 $17,449.8 $25,410.9 24.3% 13.3%
DSH $44.3 $191.4 $334.2 107.9% 20.4% $1,340.9 $17,525.6 $18,988.4 261.5% 2.7%
Administration $122.6 $148.5 $140.6 10.1% –1.8% $3,152.6 $3,797.9 $5,449.4 9.8% 12.8%
Source: The Urban Institute, 1997. Based on HCFA 2082 and HCFA 64 data.

funding source for indigent health care programs. It raises funds from a
1.5 percent assessment on each hospital’s net operating revenue and from
other selected health care providers, in addition to a portion of the cigarette
tax. PMATF funds have been used to finance Medicaid eligibility expansions,
disproportionate share hospital (DSH) payments, and county primary care
programs.
Increases in Florida’s Medicaid expenditures, both federal and state, in the
early 1990s were similar to those at the national level—27 percent average
annual growth rates between 1990 and 1992 (table 3). These increases were
caused largely by growth in AFDC and Medicaid enrollment, in part due to the
economic recession of the early 1990s, and by the expansion of Medicaid eligi-
bility to additional groups. Average annual growth rates in the state’s Medicaid
spending between 1992 and 1995 dropped significantly—to 13.4 percent on
average—but were still in excess of the national average of 9.9 percent during
that period. This higher-than-average spending was primarily due to much
greater spending increases in long-term care, primarily for the elderly. As a
percent of total 1995 expenditures, Florida spent more on acute care than the
national average (64 percent versus 50 percent), less on long-term care (28 per-
cent versus 34 percent), and less than half as much on DSH payments—5 per-
cent versus 12 percent.
The average growth in Medicaid expenditures per beneficiary in Florida
from 1992 to 1995 was 7.0 percent versus 5.5 percent for the United States as a
whole, and the excess rate of growth appeared to be concentrated on the elderly
and children (table 4). Nonetheless, the level of Medicaid expenditures per
enrollee was 16.1 percent below the national average in 1995. Largely because
of low levels of long-term care spending, expenditures per enrollee for the
elderly and disabled were 20.0 percent and 28.1 percent below the national
average, respectively. Average expenditures per child enrollee were 15.4 per-
cent above the national average.
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
14
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
THE URBAN
INSTITUTE
15
Table 4 Medicaid Expenditures per Enrollee by Eligibility Group, Florida and United States
Florida United States
Spending per Average Annual Spending per Average Annual
Enrollee Growth Enrollee Growth
1990 1992 1995 1990–92 1992–95 1990 1992 1995 1990–92 1992–95
Total $2,099 $2,195 $2,686 2.2% 7.0% $2,397 $2,729 $3,202 6.7% 5.5%
By Group
Elderly $5,300 $6,277 $7,793 8.8% 7.5% $6,839 $8,422 $9,738 11.0% 5.0%
Cash 3,086 3,175 3,585 1.4% 4.1% 3,329 4,017 4,818 9.8% 6.2%
Noncash 8,061 9,612 11,902 9.2% 7.4% 10,377 12,192 13,521 8.4% 3.5%
Blind and Disabled $4,251 $5,475 $5,767 13.5% 1.8% $6,378 $7,320 $8,022 7.1% 3.1%
Cash 3,785 5,060 5,535 15.6% 3.0% 4,969 5,927 6,686 9.2% 4.1%
Noncash 7,765 7,820 6,801 0.3% –4.5% 12,047 12,574 12,660 2.2% 0.2%
Adults $1,417 $1,252 $1,250 –6.0% 0.0% $1,301 $1,518 $1,728 8.0% 4.4%
Children $790 $993 $1,360 12.1% 11.0% $770 $931 $1,178 9.9% 8.2%
Source: The Urban Institute, 1997. Based on HCFA 2082 and HCFA 64 data.

Organizational Structure of
State Health Programs
T
he state has undergone several reorganizations of its health and human
services programs during this decade. Prior to 1992, the Department
of Health and Rehabilitative Services (DHRS) housed all health pro-
grams, including Medicaid, public health, and mental health, as well
as welfare and a range of other social service programs. In the Health Care
Reform Act of 1992, the state removed Medicaid from this enormous umbrella
department and placed it in the newly created Agency for Health Care
Administration, which reports to the governor. AHCA also has authority over
a number of health regulatory functions, including hospital budget review,
licensing and regulation of health facilities (including certificate of need), and
health care–related professional licensure. Furthermore, it oversees health care
purchasing for state employees and the newly created CHPAs for small firms
and self-employed individuals seeking coverage. DHRS retained authority over
public health and mental health in addition to other health-related programs
such as Children’s Medical Services, which operates clinics and coordinates
services for 80,000 children with disabilities throughout the state.
8
By 1996, the arrangement of health and social services was once more found
to be unsatisfactory. DHRS was still an immense human services bureaucracy,
and many believed that public health was being shortchanged. Thus, the state
created a separate Department of Health, which was given responsibility for the
divisions of family health, environmental health, and disease control, as well as
Children’s Medical Services from the former DHRS. At the same time, DHRS
was given a new name: the Department of Children and Family Services. It
still has control over Medicaid eligibility rules, as well as the mental health,
substance abuse, and developmental disability programs.

Florida’s 67 counties are responsible for administering health services pro-
grams. Each county operates a county public health unit, which is an adminis-
trative and delivery unit of the state Department of Health. While local health
department directors report to the county commissioners, county health depart-
ments are essentially state franchises; in fact, all staff are employed by the state.
Nonetheless, decisions regarding the types of services to be provided and how
to provide them are determined by each county public health unit. Nearly all of
the state’s 67 counties supplement the funds received from the state to support
their county public health department, though the amount varies tremendously
by county. Counties also share in the financing of Medicaid; they pay $55 per
month for each nursing home resident and 35 percent of the nonfederal share
for inpatient days 13 through 45.
9
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
18
Assessing the New Federalism:
Potential State Responses
to Additional Flexibility
and Reduced Funding
General State Philosophy toward the Poor
G
overnor Chiles has made a concerted effort to expand health insurance
coverage for low-income people. But in a state that has built-in limits
on tax revenues, a tax expenditure cap, and a fiscally conservative leg-
islature, he has had to settle for less than his ambitions. The legislative
agenda in 1996 was dominated by a debate over funding priorities, which was
cast as a trade-off between social and health services on the one hand and edu-
cation and corrections on the other. As in the previous year, the legislature
explicitly took funds proposed for Medicaid and transferred them to corrections
and education. There is concern in the legislature over Medicaid spending
growth and its impact on expenditures for education, job creation, economic
development, and criminal justice. In recent years, policymakers have resisted
expanding entitlements and have made regular attempts to constrain growth
in the Medicaid program. Perhaps because Medicaid eligibility and benefits
are lower than the national average, there has been little concern about attract-
ing out-of-state low-income residents.
It was surprising not to find greater support for long-term care spending,
which seems inconsistent with the large number of elderly who make up the
state’s electorate. Interviewees attributed this apparent contradiction to the fact
that many elderly have higher incomes or assets that shield them from reliance

on publicly supported services. The predominance of Latinos, whose culture
expects families to take care of their elderly parents, may also be a factor.
Medicaid-Specific Issues
According to a spokesperson for the governor, the per capita Medicaid
spending cap proposed by President Clinton earlier in 1997 would be accept-
able if it gave the state some additional flexibility to run its Medicaid program.
In particular, the state would like to be less subject to the federal courts, which
are “acting as legislators.” The spokesperson also indicated that the state has
applied for a number of waivers, some of which have been under considera-
tion by the Health Care Financing Administration (HCFA) for a long time. If
the state had not had to obtain approval for these waivers, it might have been
able to implement some innovative and potentially cost-saving programs more
quickly.
Some sources said the state wanted to have the Boren amendment
10
repealed, as some of the Boren-related suits have forced the state to pay more
than it would have liked on a number of occasions. Others agreed that a repeal
of the Boren amendment would help the state most by relieving it from having
to fight provider lawsuits, though rates would probably not change significantly.
Florida has not been as aggressive as some other states in maximizing fed-
eral funds. The state has not “abused” provider taxes and DSH spending as
much as other states have done, according to many sources. However, the state
continues to lobby extensively at the federal level to ensure “that Florida
receives a more equitable share of available federal assistance.”
11
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
20
Providing Health Coverage for
Low-Income People
Medicaid Eligibility
F
lorida is less generous in its eligibility standards for Medicaid than the
average state; in 1994, 39.6 percent of the low-income population below
150 percent of the FPL had Medicaid coverage, compared with 51 per-
cent nationally.
12
Under Florida’s Medicaid program, families with chil-
dren receiving AFDC, intact families with children, and families with unem-
ployed parents are eligible for coverage if their family income is below 28
percent of the FPL; the national average for eligibility is 41.9 percent of the FPL.
Florida has taken advantage of the option to cover pregnant women and infants
up to 185 percent of the FPL, and it has a medically needy program that covers
individuals whose medical expenses bring their income down to 28 percent of
the FPL (though the state could have extended this to 37 percent of the FPL
but did not). In addition, Florida Medicaid covers aged and disabled individu-
als with incomes up to 90 percent of the FPL and has an institutional care pro-
gram that provides nursing home and ICF/DD services to individuals with
incomes up to 300 percent of the SSI standard.
Table 5 shows that Medicaid enrollment increased from 1.2 million in 1990
to 1.8 million in 1992 (a 23.3 percent increase per year) and to 2.2 million by
1995 (another 6.2 percent increase per year). Increases in Medicaid-AFDC
enrollment averaged 24.9 percent per year between 1990 and 1992; it slowed
dramatically thereafter, averaging only 2.9 percent per year between 1992 and
1995. Medicaid-SSI enrollment grew by 8.4 percent per year from 1990 through
1995. By far the greatest increases in enrollment occurred as a result of
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
22
Table 5 Medicaid Enrollment by Eligibility Group, Florida and United States (Enrollment in Thousands)
Florida United States
Average Annual Average Annual
Enrollment Growth Enrollment Growth
1990 1992 1995 1990–92 1992–95 1990 1992 1995 1990–92 1992–95
Total 1,186.3 1,803.4 2,159.3 23.3% 6.2% 28,856.7 35,765.1 41,672.0 11.3% 5.2%
By Group
Elderly 167.4 195.9 225.2 8.2% 4.8% 3,412.2 3,771.0 4,116.6 5.1% 3.0%
Cash 92.9 101.5 111.3 4.5% 3.1% 1,713.1 1,739.2 1,789.2 0.8% 1.0%
Noncash 74.5 94.4 113.9 12.6% 6.5% 1,699.1 2,031.8 2,327.3 9.4% 4.6%
Blind and Disabled 183.3 232.4 330.9 12.6% 12.5% 4,040.9 4,875.1 6,405.2 9.8% 9.5%
Cash 161.9 197.5 270.2 10.5% 11.0% 3,236.8 3,853.4 4,973.5 9.1% 8.9%
Noncash 21.4 34.9 60.8 27.6% 20.3% 804.1 1,021.7 1,431.7 12.7% 11.9%
Adults 261.3 348.6 404.6 15.5% 5.1% 6,738.7 8,373.3 9,584.2 11.5% 4.6%
Cash 159.0 237.4 278.3 22.2% 5.4% 4,651.6 5,342.5 5,441.4 7.2% 0.6%
Noncash 102.3 111.2 126.2 4.2% 4.3% 2,087.2 3,030.9 4,142.8 20.5% 11.0%
Children 574.3 1,026.5 1,198.6 33.7% 5.3% 14,664.9 18,745.7 21,566.0 13.1% 4.8%
Cash 381.7 606.7 641.9 26.1% 1.9% 9,946.2 11,281.8 11,314.6 6.5% 0.1%
Noncash 192.6 419.8 556.7 47.6% 9.9% 4,718.7 7,463.9 10,251.4 25.8% 11.2%
Source: The Urban Institute, 1997. Based on HCFA 2082 data.

expanded eligibility groups—AFDC-UP, the medically needy program, poverty-
related pregnant women and infants (up to 185 percent of the FPL) and chil-
dren, optional coverage of elderly and disabled populations, qualified Medicare
beneficiaries, and specified low-income Medicare beneficiaries, which com-
bined to account for 44 percent of the increase in the total Medicaid caseload.
Among these groups, the largest increase, both in percentage terms and actual
numbers, was for poverty-related children. State data indicate that average
monthly caseloads for this group grew from 65,277 in FY 90–91 to 220,918 in
FY 96–97—an increase of 238 percent, accounting for more than 58 percent of
the growth in expanded eligibility groups.
13
The improved economy appears to have contributed to declines in average
monthly caseloads over the past three years. Average monthly Medicaid cases
dropped from a high of 1.6 million in FY 93–94 to 1.5 million in FY 96–97.
The improved economy has also been reflected in declines in Medicaid-
related AFDC caseloads, which went from a high of 832,942 people in
FY 93–94 to 738,955 in FY 95–96, and was projected to fall below 650,000
in FY 97–98.
The state received approval of its Section 1115 waiver application in 1994.
That program, had the legislature authorized it, would have subsidized private
health insurance to uninsured people earning up to 250 percent of the FPL who
were without coverage for the previous 12 months or had just left Medicaid.
Health insurance would have been available through the CHPAs. The state pro-
posed to finance this expansion in eligibility through savings from enrolling
more people in Medicaid managed care plans and from phasing out the med-
ically needy program, decreasing institutional provider rates, and reducing
DSH payments. An estimated 1.1 million persons could have enrolled, accord-
ing to projections. One of the major objections to the program in the Senate
(the bill was passed by the House but not the Senate) was that the income level
was too high, leading to “middle class welfare.”
14
The state’s welfare reform program is called WAGES (Work and Gain
Economic Self-sufficiency). It builds on the previous Family Transition Program
(FTP), which began in 1993 as a two-county pilot project in Alachua and
Escambia Counties. Under the pilot project, most AFDC recipients had a two-
year time limit for cash assistance and were allowed to keep more of their earn-
ings in order to create savings accounts. The project also broadened eligibility
in JOBS (Job Opportunity and Basic Skills) participation, and offered case man-
agement support to families.
Consensus that FTP’s approach was the right direction for the state resulted
in 1996 legislation authorizing WAGES. WAGES put stricter limits on the time
recipients were allowed to receive cash assistance. It also placed a 48-month
lifetime limit on benefits, required adults to work or engage in work-related
activities as a condition of receiving benefits, established immediate sanctions
for people who do not comply with work requirements, and required teen par-
ents to live at home under adult supervision and stay in school.
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
THE URBAN
INSTITUTE
23
The Department of Children and Family Services is responsible for recom-
mending policies related to Medicaid under the federal welfare reform law. The
state has an integrated eligibility system to assure that all TANF recipients will
be enrolled in Medicaid. Several interviewees believed that the biggest chal-
lenge for welfare reform would be a national economic recession: They thought
that Florida would then be more seriously affected because during economic
hardship, people who are unemployed often move from cold areas to places
like Florida, where it can be cheaper to live. At the same time, few in the state
were worried about state welfare benefits serving as an attraction to those from
out of state; these benefits are already near the bottom relative to other states
and are expected to remain there.
Other Public Financing Programs
Florida does not have a statewide General Assistance program, and thus it
has no General Assistance medical program either. Only one state program
other than Medicaid provides assistance to low-income, otherwise uninsured
people—the Healthy Kids Program.
The Healthy Kids Program is a school enrollment–based insurance pro-
gram that provides comprehensive health insurance coverage to approximately
39,300 school-aged children and their younger siblings as of August 1997.
15
The
program has won national awards for innovation in government, and the Robert
Wood Johnson Foundation has recently committed a significant amount of
funds to help other states replicate the program. It began in 1991 as a three-
year Medicaid Section 1115 waiver demonstration, financed with state and
federal funds. When the demonstration ended, federal financing also stopped;
as of FY 96–97, the program relies on financing from the state (about 49 per-
cent), participating families (about 35 percent), and local governments (about
16 percent).
16
As of this writing, the Healthy Kids Program is operating in 17 counties
throughout the state (an increase from 9 counties in the previous year), covering
approximately half of the uninsured children in the state.
17
To participate, local
school districts, which in Florida correspond to counties, must contribute an
increasing share of total program costs over time, usually obtained from ad
valorem taxes.
All school-aged children and their younger siblings are eligible for the
Healthy Kids Program. Of participating children, 71 percent come from house-
holds with incomes below 133 percent of the FPL; 15 percent, from house-
holds with incomes between 134 and 185 percent of the FPL; and 14 percent,
from households with incomes above 185 percent of the FPL. The Healthy Kids
Program encourages parental responsibility by requiring families to contribute
to the costs of providing health insurance for their children. Each local area
develops a sliding-scale premium schedule, with eligibility for reduced premi-
ums tied to eligibility for the free- and reduced-lunch programs. There are also
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
24
copayments for some services. The average monthly cost of the Healthy Kids
Program is $51.00. Participating health plans are selected based on competi-
tive bids, and only one health plan is chosen in each county.
In 1996, Governor Chiles requested $36 million for Healthy Kids from the
legislature and received $13 million to expand the program. In 1997, he
requested and received an additional $16 million, which will expand the pro-
gram to serve a total of 60,000 children. (This averages $450 per child, less
than the average cost of the program because of (1) local government and family
contributors and (2) differences in the expected costs of the new target popula-
tion.) In addition, the legislature granted ACHA the authority to seek a Section
1115 waiver to cover children with incomes up to 185 percent of the FPL
through the Healthy Kids Program. According to Healthy Kids officials, if this
waiver is approved, it would allow the program to cover 118,000 children and
thus 15.7 percent of the state’s estimated 750,000 uninsured children.
Insurance Reforms
Florida’s health insurance reforms were enacted as part of the 1992 and
1993 health care reform laws. Both laws regarded reform of small-group health
insurance as an important component of promoting competition in health care
and using managed care to achieve cost savings. The 1992 law defined small
groups as including 50 employees or less, and all insurers offering policies to
small groups were mandated to offer basic and standard benefit plans defined
by the Department of Insurance. The 1993 law required all insurers offering
policies to small groups to guarantee issue of policies without regard to health
status, preexisting conditions, or claims history; provided portability of plans
between employers; and required the use of modified rating on all small-group
products, with adjustments allowed for age, gender, family composition,
tobacco usage, and geographic location. Neither law affected the individual
market.
Since 1993, there has been no legislative action with respect to insurance
reform in the small-group or individual market. At the time of the site visit,
Florida legislative staff were working to implement an alternative mechanism
for the individual insurance market portability reforms to meet federal provi-
sions of the Health Insurance Portability and Accountability Act. According to
respondents, the state had two options: (1) Mandate that group or individual
carriers offer coverage, or (2) Reopen the state’s high-risk pool.
18
Group insur-
ance carriers were prodding individual market carriers to offer some products,
while individual carriers were trying to convince the state to reopen its high-
risk pool.
As part of its “managed-competition” health care reform laws, Florida cre-
ated 11 regional Community Health Purchasing Alliances in 1993 as state-char-
tered, nonprofit private purchasing organizations. CHPA membership is avail-
able to, though not mandated for, firms that have 50 or fewer full-time
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
THE URBAN
INSTITUTE
25

employees, including the self-employed. All policies provided through the
CHPAs must be issued through an insurance agent. In 1995, there were 64 reg-
istered carriers in the small-group market.
19
Forty are designated as
Accountable Health Plans (AHPs), which are allowed to offer HMO, preferred
provider organization (PPO), point-of-service (POS), and extended provider
organization (EPO) products through the CHPAs. Since the inception of CHPAs,
there has been significant growth in the number of individuals covered; by
January 1997, 18,000 small businesses were participating, representing more
than 76,000 covered lives.
20
Though the program does not directly subsidize
insurance premiums, slightly less than half of the 76,000 enrollees were previ-
ously uninsured. This proportion is higher than that in other states’ purchas-
ing cooperatives for small businesses—almost double that in the Health
Insurance Plan of California, for example—because Florida allows groups of
one (the self-employed) to enroll.
Despite the potential of CHPAs to lower uninsurance rates among small
firms, several factors limit their ability to provide more affordable insurance.
According to the Florida Office of Program Policy Analysis and Government
Accountability (OPPAGA), CHPAs may suffer from adverse selection; that is,
those who need insurance because they have medical conditions are more
likely to purchase it.
21
The majority of enrolled firms had only one to two
employees, whereas only 1 percent had 20 to 50 employees. This suggests a
fair amount of adverse selection, leading insurers to charge higher premiums. In
addition, CHPAs are prohibited from negotiating rates with insurers so that the
CHPAs cannot take advantage of their market power. Because of these factors,
premiums for CHPA-sponsored insurance plans were only about 6 percent less
than premiums for the same plans offered outside of the CHPAs, according to a
1995 report commissioned by OPPAGA. This is less than the cost advantage
expected for group purchasing.
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
26
Financing and Delivery System
F
lorida’s health care market is one of the most competitive and entre-
preneurial in the country. Most HMOs are for-profit and are in a period
of instability; mergers and acquisitions are occurring at a fast pace. In
addition, more hospitals are for-profit than in most other states. There
has been little apparent public concern over issues raised by conversions from
nonprofit to for-profit status. However, the recent emergence of alliances
between public hospitals and investor-owned organizations and the potential
conversion of some of the bigger public hospitals to private ownership (such
as Tampa General) are likely to increase interest in this issue.
Hospitals, and in particular hospitals in the larger systems, are faring rela-
tively well, perhaps because of the large Medicare market. (Medicare is gener-
ally seen as a better payer than private managed care plans.) The hospital indus-
try remains over-bedded, which means that HMOs can still negotiate significant
discounts. Safety net institutions are in relatively good financial health, in large
part because of local financing arrangements that exist in many of the metro-
politan areas with large low-income populations.
Commercial Managed Care
Commercial managed care has been growing rapidly in Florida, as more
purchasers of health care switch to managed care as a lower cost insurance
alternative. As of 1995, 25 percent of the state’s population was enrolled in an
HMO.
22
HMO market penetration, however, varies considerably across the state.
Tallahassee, dominated by state employees who have incentives to enroll in
managed care plans, has the highest HMO penetration, at 42.1 percent. Dade
County has the second highest, at 40.8 percent, and the Tampa–St. Petersburg

area has approximately 28.1 percent HMO penetration. As of 1992, 26.7 percent
of the state’s population was enrolled in a PPO.
Enrollment in commercial managed care is concentrated in a few HMOs. As
of 1996, 10 HMOs accounted for approximately 81 percent of commercial
enrollment, and 5 HMOs (Blue Cross/Blue Shield’s [BC/BS] Health Options,
Humana Medical Plan, United Health Care Plans of Florida, Prudential Health
Care Plan, and Cigna) accounted for almost 60 percent of the market.
The Florida HMO market has been a profitable one, but it has become less so
in the last few years, particularly for the smaller HMOs. In 1995, with a few
exceptions, the top 10 HMOs fared quite well, recording net revenues in excess
of $125 million, or 86 percent of total HMO profits.
23
The remaining 28 HMOs,
with approximately 20 percent of the market, garnered only 14 percent of the
profits. More recent data show that about half of the state’s HMOs had losses
in the last quarter of 1996. Medicaid HMOs showed particular signs of financial
distress as state rate reductions and increasing competition have made their
margins much smaller. Consolidation in the market is expected, as smaller,
struggling HMOs are attractive acquisitions for larger Florida-based and
national HMOs.
In the last decade, state policy has generally favored the growth of man-
aged care. Yet, as in the rest of the country, the last two years have seen a spate
of new legislation to regulate managed care. In 1996, the state enacted Senate
Bill (SB) 886, which included a number of changes to state regulations of man-
aged care organizations. First, the bill required the Department of Insurance to
publish the medical loss ratios of all plans, although there continues to be
debate around how to categorize certain expenses (medical expense vs. admin-
istration and profit). SB 886 also required HMOs to pay for emergency room
screening tests that are consistent with symptoms. The law further required a
minimum length of stay for maternity cases.
At the time of our visit, the 1997 legislative session appeared likely to see
another round of legislation. According to the Florida Association of HMOs
(FAHMO)
24
and state legislative staff, likely bills included greater access to
certain specialists; prohibitions on gag clauses (though most HMOs have
already adopted the “patient rights” principles of the American Association of
Health Plans); requirements that HMO medical directors be licensed in Florida;
written standards on referrals, quality, and access indicators; uniform cus-
tomer satisfaction surveys; establishment of an early and periodic screening,
diagnosis, and treatment (EPSDT) target of 90 percent versus the current rate
of 60 percent for Medicaid HMOs; expedited grievance procedures; medical
necessity processes; provider credentialing requirements; and ownership of
patients’ medical records by physicians.
25
None were considered by FAHMO
to be worth a serious fight, given the negative publicity that HMOs have been
receiving. There have been concerns about HMO quality, especially among
Medicaid HMOs. (These issues are discussed below in the Medicaid managed
care section.)
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
28
Hospital Market and Regulatory Issues
The Florida hospital market is considered over-bedded. As of 1996, hospi-
tals averaged only a 51 percent occupancy rate.
26
The competitive pressures
exerted on hospitals by HMOs and other managed care plans through negoti-
ated discounts have forced hospitals to change rapidly. Their responses have
included consolidating through acquisitions and mergers to attain greater effi-
ciencies and market leverage, aligning with physicians either in physician-
hospital organizations that can contract with managed care plans or buying
physician practices outright, developing or becoming part-owner in an HMO,
and attempting to convert acute care beds to subacute or nursing-care beds.
It is in this last area that state policy has been most influential. The state’s
certificate-of-need program—which attempts to maintain nursing home occu-
pancy rates at 91 percent—makes redeploying excess acute beds to nursing-care
beds difficult. The nursing home industry has fought the hospital association’s
attempt to deregulate conversion of beds from acute to subacute, leading to
legislative defeats for hospitals in both 1995 and 1996. Both sides agreed that
it could once more become a legislative issue in 1997.
Mergers and For-Profit Conversions
Reflecting trends in the rest of the country, Florida HMOs are consolidat-
ing through acquisitions and mergers. In total, there were 18 mergers or acqui-
sitions between 1993 and 1996.
27
Most of the big HMOs in Florida are mem-
bers of national chains. Hospitals also have been consolidating, and in the
process, the hospital market in Florida has changed from one of independent
hospitals to one dominated by several large hospital systems. According to the
Florida Hospital Association, 77 transactions have occurred involving an acqui-
sition or merger of a hospital or group of hospitals since 1990, peaking in 1994.
By 1996, 76 percent of the beds and hospitals were in a hospital system. The
resultant market is dominated by three hospital systems, Columbia/HCA, Tenet
HealthCare, and Adventist Health System/Sunbelt, which together account for
45 percent of the hospitals and beds in the state. While for-profit systems have
been driving the consolidation movement, nonprofit systems are growing as
well. Although consolidation activities have been high, the actual impact on the
number of hospitals and beds has been relatively small. Between 1990 and
1995, a net reduction of only 213 acute-care hospital beds occurred.
An interesting development in Florida has been the discussion or formation
of joint ventures and coalitions between public and for-profit institutions.
Public hospitals in both Jacksonville and Miami have proposed or discussed a
joint venture with Columbia/HCA. The University Medical Center in Jackson-
ville has planned to enter into an operating agreement with for-profit Columbia/
HCA to operate the hospital. The joint venture would continue to provide city-
sponsored care but would be operated by Columbia/HCA. Interviewees in
Miami indicated that Jackson Memorial Hospital had approached Columbia/
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
THE URBAN
INSTITUTE
29

HCA regarding a potential relationship, which had yet to be disclosed. Tampa
General has proposed privatization, though it is not clear whether or not this
would be in partnership with an existing private entity.
The state attorney general’s office has taken an interest in such deals
because of the potential loss of community assets. The attorney general filed a
motion (Butterworth v. University Medical Center) in 1996 after the University
Medical Center (UMC) in Jacksonville refused to provide documents regarding
the relationship between UMC and Columbia/HCA. The attorney general’s
office is also deciding whether or not it should review Tampa General’s priva-
tization plan.
At the same time that the attorney general’s office and consumers are wor-
ried about the loss of community assets, Columbia/HCA and the South Florida
Hospital Association have publicly challenged the tax-exempt status of non-
profit hospitals that they argue provide little community benefit. A 1994 pro-
posed bill would have required nonprofit hospitals either to provide more than
3.7 percent of revenues in charity care and bad debt or to pay the state’s 6 per-
cent sales tax. The South Florida Hospital Association is currently gathering
data on the community benefits provided by nonprofit hospitals to determine
whether or not they equal or exceed the tax benefit the hospitals receive.
Medicaid Provider Reimbursement
(including DSH Payments)
While Florida has moved to enroll more Medicaid enrollees in capitated
managed care, at the time of the site visit, the majority of hospital and physician
services were provided on a fee for service (FFS) basis through the state’s pri-
mary care case management program, MediPass. Thus, although the importance
of FFS reimbursement may wane in the future, a significant portion of hospital
and physician services is still reimbursed on an FFS basis.
The generosity of Medicaid hospital FFS payments in Florida relative to
the rest of the nation has declined. According to data from the American
Hospital Association, for the nation as a whole, Medicaid payments as a percent
of costs increased considerably, from 78 percent in 1989 to 93 percent in 1993.
In Florida, however, the ratio remained relatively constant at 82 to 83 percent,
changing only one percentage point between 1989 and 1993.
28
Nonetheless, rep-
resentatives from the state hospital association and various hospitals indicated
that the level of Medicaid payments was not viewed as a serious problem
because competition has driven down private rates to the point where Medicaid
rates appear good. Currently, no Boren amendment suits are being brought
against the state by hospitals.
Compared with other states, Florida has a relatively modest disproportion-
ate share hospital program, spending about $334 million in 1995 (table 3) and
$369 million in FY 96–97. As of 1995, DSH spending represented only
5 percent of total Medicaid spending, considerably lower than that for the
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
30

United States as a whole (12 percent). Moreover, since 1992, DSH has remained
at approximately 5 percent of total state Medicaid expenditures.
Florida currently maintains five DSH programs: (1) regular DSH, which pro-
vides payments to those hospitals that treat a disproportionate share of charity
and Medicaid patients; (2) mental health DSH for hospitals that serve patients
requiring psychiatric services, regardless of their ability to pay; (3) a DSH pro-
gram that supports graduate medical education; (4) DSH payments to regional
perinatal intensive care centers (RPICCs), which have exceptionally high costs
or long lengths of stay for infants; and (5) rural hospital DSH payments. As of
FY 96, the mental health DSH program was the largest component (49 percent),
followed by the regular program (41 percent), teaching hospitals (5 percent),
rural hospitals (2 percent), and the RPICCs (2 percent).
29
The regular DSH program began in 1988 and was funded largely through
provider taxes, which were deposited into the Public Medical Assistance
Trust Fund, and general revenues. In 1990, state lawmakers expanded the
Trust Fund’s revenues by increasing the cigarette tax; in 1991, by expanding
the base to include ambulatory surgical centers, clinical laboratories, free-
standing radiation therapy centers, and diagnostic imaging centers; and in
1992, by imposing a $1.50 assessment for each patient-day provided by nurs-
ing homes. Between 1988 and FY 92–93, some of these funds were used to
leverage federal funds and provide specific hospitals—those that treated a
high percentage of Medicaid and indigent patients—with additional revenues.
These funds were also used to support graduate medical education (begun in
FY 91–92), RPICC (begun in FY 89–90), and rural hospital DSH programs
(begun in FY 93–94).
In response to changes in DSH rules contained in the federal Omnibus
Budget Reconciliation Act of 1993 (OBRA 93), the state created a new inter-
governmental transfer program to help finance DSH payments. To pay for the
regular DSH program, a few publicly owned hospitals provide the lion’s share
of state revenues through intergovernmental transfers. As of 1993, approxi-
mately $88 million in intergovernmental transfers came from Dade, Duval, and
Hillsborough Counties.
30
According to state officials, the eligibility criteria and
payment formulas were designed so that the large public hospitals in these
counties receive a significant portion of regular DSH monies. As a result, the
three hospitals receive about 81 percent of the state’s regular DSH dollars, and
all other DSH-qualifying hospitals receive the rest.
In further response to OBRA 93, the state aggressively expanded its mental
health DSH program, managing to spend up to the allotment allowed under
OBRA legislation. The state transferred approximately $81 million that was pre-
viously used to fund the state-owned mental health institutions to the DSH pro-
gram to draw down federal matching funds. Although the mental health DSH
program represented only 27 percent of DSH in FY 92–93, it has been a vehi-
cle for growth in DSH. By FY 96–97, the mental health DSH program accounted
for almost 50 percent of total DSH expenditures.
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
THE URBAN
INSTITUTE
31

As of 1993, Medicaid physician fee levels in Florida were roughly equiva-
lent to the national average Medicaid fee levels and 78 percent of Medicare fees.
Between 1990 and 1993, fees for obstetric services increased considerably. For
example, the fee for a vaginal delivery increased by 60 percent, while a com-
mon primary care visit increased by only 7.5 percent. Between 1993 and 1996,
fees increased by over 80 percent for the same primary care visit, while obstet-
ric fees remained the same.
31
Changes in fee levels in Florida between 1993 and 1996 were largely dri-
ven by the implementation of the Medicare resource-based relative-value scale
(RBRVS). The state’s Medicaid program began reimbursing physicians using the
RBRVS in 1995. The state maintained budget neutrality by creating a conver-
sion factor that led to no change in total expected expenditures for physician
services. The movement to RBRVS shifted 10 percent of expenditures from
medical and surgical specialty visits to evaluation and management visits.
Since that time, there have been few changes in physician fees.
Recently, the governor has recommended an across-the-board reduction in
fees to fund retroactive payments to physicians who successfully sued the state
because they had been paid the Medicaid rate rather than the Medicare rate for
their services to dual eligibles. The governor has recommended a reduction in
the conversion factor that would cut rates by an average of $7.09 per procedure.
This amount represents approximately 19.2 percent of the $453 million bud-
get for physician services expenditures.
32
Medicaid Managed Care
Florida’s history with Medicaid managed care dates back to 1977, when
the legislature granted authority to the Medicaid agency to contract with HMOs.
However, there was little interest on the part of HMOs. In 1978, Medicaid also
obtained authorization to contract with county public health units on a prepaid
basis, which resulted in one demonstration program in Palm Beach County. The
pace of managed care contracting picked up in 1983, when the legislature
authorized Medicaid to contract with prepaid health plans (PHPs), which are
health care organizations that accept capitation payment but, as federal law per-
mits, do not have to obtain a state HMO license until three years from the start
of the contract. The state contracted with four PHPs. Despite efforts to solicit
interest among plans on a case-by-case basis, by 1989 the state still had no con-
tracts with commercial HMOs, and there were only about 50,000 enrollees in
PHPs out of about 900,000 total beneficiaries.
Further Medicaid HMO growth was spurred through state policies in the
early 1990s that made it easier for HMOs to enter the market. Among the most
important policies were those allowing door-to-door marketing, as well as mar-
keting in welfare and food stamp offices; establishing relatively generous rates,
based on 95 percent of FFS payments, which in turn were higher because of
updated fee schedules; and lowering capitalization requirements for PHPs to
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
32

only $250,000 in reserves. These changes led to a substantial increase in small
PHPs and HMOs contracting with Medicaid—14 in 5 counties by 1990 and 29
in 48 counties by 1995. Many of the HMOs were out-of-state companies that got
their start by acquiring small Medicaid PHPs.
In 1991, the state launched a primary care case management (PCCM) pro-
gram called MediPass. Like many other PCCM programs, it pays a $3.00
monthly case management fee to physicians or clinics to coordinate all the
care for patients and to authorize all services, which continue to be paid on a
FFS basis. While some assert that AHCA developed MediPass because not
enough HMOs would participate in Medicaid, others believe that MediPass pro-
vides enrollees with an alternative to HMOs and ensures that HMOs have some
competition.
The state passed a law in April 1993 that required enrollment in managed
care for much of the Medicaid population. As a result, the state began efforts
to implement MediPass in all areas of the state. The state submitted a revised
1915(b) waiver proposing statewide expansion, which was subsequently
approved by HCFA.
The state’s passage of the 1993 law requiring mandatory enrollment in some
type of managed care program was driven by two forces. The most important
was budgetary. With annual Medicaid program growth rates in the 20 percent
range, the legislature was desperately seeking relief, and managed care seemed
to hold the key to cost savings for the nonelderly population.
33
Second, AHCA
believed that expansion in managed care and the resulting savings were essen-
tial to financing the Florida Health Security Program. Although the legislature
turned down Florida Health Security’s proposed eligibility expansion, partly
because of concerns that managed care savings might not be sufficient to cover
all those eligible, it still wanted to harness some of the savings to hold down
annual growth rates.
Enrollment
As a result of state policies and successful HMO marketing tactics, Florida’s
Medicaid managed care market grew rapidly between 1991 and 1995.
34
In 1991,
about 123,000 (13 percent) Medicaid beneficiaries were enrolled in some form
of managed care: HMOs, PHPs, or the MediPass program. By 1996, nearly one
million (66 percent) Medicaid beneficiaries were enrolled in some form of man-
aged care. As a result of the 1995 enrollment freezes and rate reductions, how-
ever, enrollment in Medicaid HMOs or PHPs actually dropped between 1995
and 1996 by about 37,000, and the number of Medicaid HMOs or PHPs dropped
from 29 in FY 94–95 to 19 in FY 96–97. Enrollment in the MediPass program
has increased every year because of the 1993 mandate to implement the pro-
gram in every county.
Until recently, the state’s 1915(b) waiver allowed statewide mandatory
enrollment in MediPass of all newly eligible AFDC and SSI populations (or
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
THE URBAN
INSTITUTE
33

those coming back onto Medicaid after a 90-day exit period), if they do not
choose to enroll in an HMO or PHP. This recently changed, however, as a result
of SB 886, the law passed in 1996 that allows the state to mandate assignment
into either MediPass or an HMO or PHP. Effective February 1, 1997, the state
began assigning new AFDC-related enrollees according to a ratio established
in SB 886: 60 percent of those who do not select either program voluntarily will
be assigned to HMOs or PHPs and 40 percent, to MediPass.
35
SSI recipients
were to be assigned starting May 1, 1997 (and notified of the requirement to
choose or be assigned on March 1, 1997). The only exceptions to mandatory
enrollment are for dual eligibles, presumptively eligible pregnant women, med-
ically needy, and those in skilled nursing facilities (SNFs) or ICFs/DD.
36
The rapid growth in Medicaid HMOs and PHPs during the early 1990s came
at some cost. In December 1994, a yearlong investigation into Medicaid HMOs
in South Florida led to a weeklong series of articles in the Fort Lauderdale Sun
Sentinel that exposed poor-quality care and flagrant marketing abuses. In
response to public outcry, the state placed a moratorium on the licensing of
any new Medicaid HMOs in January 1995. It also froze enrollment in the 28
Medicaid HMOs that were already licensed until the AHCA could conduct on-
site visits to assess plan compliance with patient medical records requirements,
quality-of-care standards, and marketing practices.
37
Based on AHCA’s findings, the state made substantial modifications to
Medicaid HMO contracts commencing after July 1995, many of which were
subsequently incorporated into law in 1996. Medicaid HMOs and PHPs are now
prohibited from door-to-door marketing, marketing in Food Stamp and AFDC
offices, “give-aways,” and subcontracts with brokerage firms or independent
agents. Plans must also submit marketing materials to AHCA for approval, and
all such materials must contain the state’s toll-free HMO complaint hotline.
Marketing commissions were limited to 40 percent of total compensation. The
state’s role in marketing and beneficiary education, which has been minimal,
will increase as a result of SB 886, which authorized a choice-counseling pro-
gram to be implemented during 1997. AHCA received $15 million to imple-
ment this program.
38
At the time of the site visit, it was developing the request
for proposal (RFP) for an enrollment broker, which would allow face-to-face
counseling and interactive kiosks.
Contracting Issues
In August 1995, Medicaid began adjusting capitation rates by age for the first
time. According to HMO association representatives, the adjustment had the
effect of reducing rates by 14 percent on average. There was a perception that
more could be squeezed from HMO/PHP rates, despite an assessment by AHCA
that the current financial status of many HMOs/PHPs is tenuous. In SB 886
and corresponding FY 96–97 budget language, the legislature set a target of
$17 million savings (out of $700 million spent annually on HMOs), by cutting
capitation rates from 95 percent to 92 percent of FFS rates. To achieve this, SB
886 mandated a competitive bidding process for HMOs, with a maximum rate
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
34
of 92 percent of FFS rates allowed, over HMO opposition. HMOs were allowed
to bid as low as 87 percent. In February 1997, 25 bidders were announced in the
notice of intent to award contracts. Among the existing contractors, only two
did not choose to submit bids. Nine new plans won awards, including Humana,
which is entering the Medicaid market for the first time in Florida. Alpha
Health Plan, composed of many of the state’s Federally Qualified Health Centers
(FQHCs), also won an award.
The legislature’s targeted level of savings for FY 96–97 is unlikely to be
achieved for two reasons. First, the law assumed that the bidding process and
awards would be made shortly after the start of the fiscal year (July 1996), but
the process took considerably longer.
39
Second, HMOs and PHPs claimed that
the rewards for low bids, that is, more enrollees, were not sufficient to make a
difference, so only one of them bid at less than 92 percent of FFS rates.
The RFP was portrayed by AHCA as the first time that contract awards
would be based on the quality of care delivered by the plans. Plans would be
awarded points, with 80 percent of the points depending on quality measures,
such as service delivery and benefit enhancements, and only 20 percent on
price.
40
Plans would be awarded more enrollee slots as the number of points
increased. Plan representatives believed the importance of quality was over-
stated, since any plan with an existing contract needed only to document its
service delivery, patient service, and quality assurance procedures. Thus, only
the new plans had to prove their ability to provide high-quality care.
Even before the contracts were signed, the plans contested AHCA’s capac-
ity limits. Bidders that scored high enough to win contracts were given “enroll-
ment capacity awards,” based on their final scores. The number of Medicaid eli-
gibles in each county as of July 1996 times 110 percent was used as the measure
of overall enrollment capacity. The state determined enrollment slots allocated
to each plan based on its share of the points awarded and the total enrollment
capacity in the county. Because points did not vary much among plans, the
result of this complicated scoring system is only a little more capacity for the
highest scoring plans than for the lowest scoring plans.
Another problem with the new contracting system is that the state’s capita-
tion rate methodology is not very sophisticated, as one AHCA official readily
admitted. As a result, if rates are set too high, HMOs may get windfall profits; if
too low, quality of care and plan solvency are threatened. AHCA would like to
implement a risk adjustment system to correct the current system’s flaws but
believes that the HMO industry will fight it. A private consultant study esti-
mated that $60 million would need to be transferred among plans to even out the
risk levels—an amount too great to be ignored. The study found that virtually
all of the difference was due to some plans having more SSI enrollees than oth-
ers. If risk adjustment occurs, it will probably have to be legislatively mandated.
Those plans that sign contracts will, for the first time, be required to be com-
mercially licensed. SB 886 requires Medicaid HMOs and PHPs to have a cer-
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
THE URBAN
INSTITUTE
35

tificate of authority from the Florida Department of Insurance or to obtain one
within a year of signing a contract. Exceptions are still made for plans owned
and operated by a county, a county public health unit, a county-owned-and-
operated hospital, or one or more FQHCs.
41
By having to obtain a commercial
HMO license, all Medicaid contracting plans are subject to greater oversight of
their financial status by the Department of Insurance, which helps AHCA mon-
itor HMO and PHP finances. Furthermore, AHCA requires all contracting plans
to maintain at least 25 percent commercial enrollment (not Medicare or
Medicaid) unless the plan has a waiver from HCFA. It was noted, however,
that even when plans have both Medicaid and commercial enrollees, they often
have separate provider networks. Thus, the 75-25 rule may not achieve what
was intended. Finally, all Medicaid contractors are required to report HEDIS 2.5
(Health Employer Data and Information Set) measures, and AHCA has also
designed a member satisfaction survey that all Medicaid HMOs and plans par-
ticipating in the CHPAs must use.
Elderly Managed Care
AHCA and the Department of Elder Affairs are trying to implement a pilot
project in Palm Beach County called the “long-term care diversion waiver.” It
involves capitation of an integrated set of long-term care and acute-care services
for 600 elderly persons. Although the program is not yet operational, the
FY 97–98 budget bill proposes a doubling of the program. Advocates and poli-
cymakers both acknowledge that the program is very limited in scope relative
to the needs of the elderly population in Florida. Nonetheless, it is considered
an important first step toward managed care for the elderly population.
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
36
Delivering Health Care to the
Uninsured Population
State and County Public Health Programs
H
istorically, county public health units in Florida served as the major
health care delivery system for the poor—Medicaid enrollees and
uninsured alike. As branches of the state health department, all
county health departments at some point provided maternal and
child health services; Women, Infants and Children (WIC) services; family
planning; and sexually transmitted disease screening and treatment. A few
county health departments provided more comprehensive primary care ser-
vices. Most of these services were Medicaid-reimbursable for Medicaid clients,
and county public health units received cost-based reimbursement for them,
according to state law. Some counties, such as Dade, have closed their pri-
mary care clinics and have shifted their focus to core public health activities,
such as communicable disease control, maternal and child health support ser-
vices, and environmental health.
Counties also have the primary responsibility for financing health care for
the poor who are ineligible for Medicaid. However, the extent of county effort
varies considerably. Since the 1930s, Florida has allowed localities (cities,
counties, and special districts) to establish special health care taxing districts.
There are currently 21 in the state. Through the establishment of the taxing
district, some cities in Florida have been able to expand their tax base to
include suburban areas, which increases the flow of money considerably. In
some cases the money raised is quite significant, representing half of all money
used to fund care for the medically indigent.
Most of the taxing districts use their revenues to support public hospitals (as
in Dade and Broward Counties), although some distribute the funds more
broadly among hospitals providing uncompensated care or to private hospitals
that have leases with the district. In Hillsborough County, the taxes are used to
support a unique program providing insurance to many of its uninsured, low-
income residents (discussed further below).
Impact of Government Policies and Market Changes on
Safety Net Providers in Dade and Hillsborough Counties
While the major safety net providers face tremendous competitive pressures,
particularly for Medicaid patients, many of the organizations visited have weath-
ered the storms of change reasonably well over the past few years. A major rea-
son for this success is an increase in local support for indigent care. In both Dade
and Hillsborough Counties, local support for indigent care has increased con-
siderably with the implementation of a half-cent sales tax in each locale. In addi-
tion, part of the success of the safety net providers stems from their ability to
adapt to the requirements of a competitive managed care environment. Hospitals
and FQHCs have developed their own HMOs or PHPs, partnered with other
HMOs and PHPs, developed networks with other health care providers to
achieve greater efficiencies, or refocused on their core missions.
Not all safety net providers in the sites visited are faring well, particularly
community clinics. In the present relatively rosy fiscal environment, how well
safety net providers have survived seems partly a function of the manner in
which increases in local funds are distributed to those providers. In Hills-
borough County, where the revenues have been used to fund systems of care
across many different types of providers, most safety net providers seem to be
doing remarkably well. In Dade County, where the revenues are centralized in
the large public hospital, some community clinics are not faring so well.
Without local subsidies, clinics have less maneuvering room in such a highly
competitive market.
Competition for Medicaid patients and potential reductions in Medicaid
reimbursement levels have raised the level of concern among safety net
providers. While increases in reimbursement and eligibility in the early 1990s
have helped safety net providers considerably, providers and advocates are
worried that planned reductions in Medicaid rates or a further loss of patients
to other providers will undermine the financial viability of the safety net
providers and will re-create the access problems that existed in the 1980s.
Safety net providers recognize that many Medicaid patients currently receive
care through other institutions when they have Medicaid coverage. However,
they are less certain that those institutions will continue to provide care to
individuals who lose their coverage. If the safety net providers fail or scale
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
38

back services as a result of losses in revenue, then at the very least, quality of
care for the uninsured (both the chronically uninsured and those who fall on
and off Medicaid or other third-party coverage) may decline. At worst, the
uninsured may be forced back into the emergency room as a primary source
of medical care.
Tampa/Hillsborough County
Hillsborough County, which encompasses the city of Tampa and the sur-
rounding suburban and semirural areas, has a population of 879,000. The mar-
ket was characterized as very competitive, with Columbia/HCA and BayCare
having emerged as major players in the hospital market. The HMO penetration
rate now stands at 25 to 30 percent, a rapid jump from 14 percent in 1994. This
increase was prompted in part by the entry of United HealthCare and Health
Plan of Florida into the market in 1993–94 and by their subsequent marketing
to small businesses that dominate the economy. Their growth has created both
pressure for hospitals to discount their fees to hospitals and tighter provider
networks.
The Hillsborough County Health Care Plan (HCHCP), which provides
health coverage to otherwise uninsured, low-income people, was developed to
reduce the double-digit growth rate in uncompensated-care costs. Before
HCHCP, $34 million in property taxes supported the county’s obligations for
indigent care, the majority of which was used to subsidize Tampa General
Hospital (TGH), a publicly owned facility. According to respondents, as a
result of a rapid rise in indigent care costs to the county (about 20 percent per
year) and to other area hospitals (about 10 percent per year), a County Board
of Commissioners advisory board recommended a plan to provide and finance
health care services for the county’s indigent population based on managed
care principles. By September 1991, the Florida legislature and the county
board approved a half-cent sales tax to finance the program, which began in
1992. In FY 95, the HCHCP spent approximately $63 million providing ser-
vices to 27,000 individuals.
42
HCHCP provides insurance coverage to a relatively small pool of individu-
als at little cost to enrollees. Individuals with income below 100 percent of the
FPL and who are not eligible for Medicaid or other health insurance are eligible
for HCHCP without any premium contributions.
43
A catastrophic plan is also
available for people earning up to 200 percent of the FPL, but it requires pre-
mium sharing. The program offers a comprehensive benefit package, including
primary care, inpatient and outpatient surgical services, mental health, dental
care, substance abuse services, and home health services. Cost sharing is lim-
ited; patients have a small copayment for prescribed medical equipment, vision
care, and dental care.
The program contracts on a risk-basis with four provider networks (one per
geographic area within the county) to provide inpatient and outpatient ser-
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
THE URBAN
INSTITUTE
39

vices to HCHCP beneficiaries within a global budget negotiated annually with
the county. Participating network providers include TGH (which participates in
all four networks), two private nonprofit hospitals, two for-profit hospitals, the
University of Florida faculty, two FQHCs, the county public health units, and
private community physicians. Enrollees are given an HCHCP card and can
choose any participating provider as their primary care physician. At the time
of eligibility review, enrollees can request a change of provider.
The HCHCP program has grown considerably since inception and has had
a significant impact on the county’s indigent care costs. From 1993 to 1995,
the caseload increased by 23 percent, from 21,000 to 27,000 patients.
Respondents estimated that the program provided coverage to 66 percent of
the population eligible for HCHCP. According to most respondents, the program
has been very successful. First, the program has redistributed the delivery of
indigent care among providers and relieved some of TGH’s indigent care load.
Second, it has reduced emergency room use by program participants by nearly
25 percent, saving the county more than $8 million.
44
Third, the program has
reduced the average length of stay by more than 30 percent, resulting in esti-
mated inpatient hospital savings of $2 million. Finally, HCHCP has expanded
the number of community care sites.
Despite its successes, the HCHCP could become somewhat unstable, given
its funding source. The significant growth in reserves (in excess of $100 million)
has led some politicians to suggest that the program does not require such
extensive tax support.
45
In the event that the tax used to fund the program is
repealed or reduced, the safety net providers could find themselves in serious
financial trouble.
The major safety net hospitals in Hillsborough County are TGH and
St. Joseph’s Hospital. Besides having a system of family care centers, TGH has
the region’s only Level 1 trauma center, two aeromedical helicopters, a regional
burn center, and many other specialty programs. TGH also owns and operates
its own Medicaid HMO, called Healthease. Over the past five years,
St. Joseph’s–St. Anthony’s Health System has grown from a single hospital to a
complete system, which also includes Women’s Hospital, Tampa Children’s
Hospital at St. Joseph’s, and other services, such as home health and diagnos-
tic centers.
TGH provides the bulk of care to the uninsured, and St. Joseph’s handles a
growing share of the Medicaid market. According to AHCA annual hospital
reporting data, TGH’s charity care in 1995 was $52.4 million; St. Joseph’s
reported $21.3 million that same year. The competition for Medicaid patients is
putting financial pressure on TGH. St. Joseph’s–St. Anthony’s Health System
now serves more of the Medicaid market than TGH. TGH reports that it went
from serving 60 percent of the Medicaid market to 30 percent (and dropped
from 5,600 to 3,000 deliveries per year). Meanwhile, St. Joseph’s went from 19
percent to 38 percent of the Medicaid market by luring pregnant women to a
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
40

newly acquired women’s hospital; it is now building a new children’s hospital
to gain more of the children’s market.
The loss of Medicaid revenue means that TGH is increasingly reliant on
state and local support and its own initiative in developing strategies to
increase the organization’s efficiency and market viability. Despite the fact
that St. Joseph’s provides a sizable amount of care to the low-income popula-
tion, TGH receives the lion’s share of public support for care for the medically
indigent. In FY 95–96, St. Joseph’s received $10,000 from the state in DSH
payments, a small fraction of the $18.3 million TGH received.
46
Other state
policies are helpful to TGH as well. For example, while TGH’s HMO
(Healthease) had only about 4,000 Medicaid members in early 1997, it was
awarded 37,000 slots in the latest Medicaid RFP process, which TGH believes
reflects an effort by the state to assist safety net hospitals. Furthermore, the
state’s certificate-of-need process prohibits the proliferation of tertiary and
quaternary services, thus protecting the interests of TGH. Locally, TGH has an
advantage because all four HCHCP geographic networks contract with TGH
for specialty services.
There are two FQHCs in Hillsborough County: Tampa Community Health
Centers (TCHC) and Suncoast Community Health Centers. TCHC opened in
1986 with one site, but it has grown to five clinical sites. Suncoast is located in
a more rural area of the county. It began as a program of the county health
department serving Hispanic migrant farm workers, and it has added two more
sites and is expanding its staff and clientele. Because of the growth in Medicaid
HMOs, Suncoast has lost 4,000 Medicaid patients in the last three years, harm-
ing its ability to provide a full range of services to its patients.
As survival strategies, the two FQHCs have become very involved in
Medicaid managed care and HCHCP. For example, both TCHC and Suncoast are
the designated “gatekeepers” for two different HCHCP networks. TCHC has
contracts with several Medicaid HMOs, yet it says it is losing money on all
these contracts. For this reason, Suncoast has not become part of one of the
leading Medicaid HMOs’ network, but nonparticipation has hurt it. To try to
regain Medicaid patients, both TCHC and Suncoast were two of 17 FQHCs in
Florida that allied to form the Alpha Health Plan. Alpha recently won a contract
in the most recent round of Medicaid HMO awards. Alpha will pay the FQHCs
better rates than other Medicaid HMOs and will also pursue commercial con-
tracts to comply with the 75-25 rule.
The Hillsborough County Health Department decided in 1994 that it would
withdraw from the HCHCP and divest from directly providing primary care ser-
vices, even though it still needs Medicaid business to support health services to
the uninsured who are ineligible (e.g., undocumented aliens) or who do not
sign up for HCHCP. The health department instead contracts with a group of
midwives and pediatricians to provide primary care to uninsured and
Medicaid-covered children and pregnant women. Most of the funds for these
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
THE URBAN
INSTITUTE
41

services are generated from Medicaid FFS payments under MediPass. The
health department also has a few Medicaid managed care contracts.
Miami/Dade County
Dade County, which includes the city of Miami and the surrounding urban
(South Beach) and suburban areas, had a population of more than 2.1 million in
1995, with 1.7 million people under the age of 65. Respondents indicated that
although access to care for low-income individuals has improved considerably
since the early 1990s, problems remain. According to advocates, a large number
of women and children are still not receiving health care services, especially
undocumented immigrants from Central and South America and Haiti. The
county has unique health problems as well, such as hanta virus, tuberculosis,
malaria, cholera, and hepatitis, which are attributable to some extent to Miami’s
status as an immigration center.
The Miami–Hialeah metropolitan area had the second-highest HMO pene-
tration rate in the state, at 37.8 percent.
47
With a bed-to-population ratio of 4.1
per 1,000, the hospital market is over-bedded. The hospital market is concen-
trated in two for-profit systems and a nonprofit hospital system. Together, for-
profit Columbia/HCA and Tenet control almost 40 percent of the beds in the
market. The Dimension System, which is technically a physician-hospital orga-
nization comprising for-profit and nonprofit hospitals, controls almost 26 per-
cent of the beds.
The county’s dominant source of care for the indigent is Jackson Memorial
Hospital, a publicly owned hospital that receives substantial subsidies from the
Dade County Public Health Trust (the public hospital taxing district). According
to Jackson Memorial officials, although the Trust and Jackson Memorial
Hospital are separate entities, they are regarded as one, since all of the Trust
funds are allocated to Jackson Memorial Hospital and its affiliated centers. The
Trust is funded through a variety of revenue streams: (1) a half-cent sales tax
that was passed by Dade County voters in September 1991 and raises $96 mil-
lion annually; (2) ad valorem taxes, which in FY 95–96, totaled $84 million;
and (3) federal and state grants, which total about $10 million annually. The
remainder of the $750 million budget is generated through DSH payments and
through commercial, Medicaid, and Medicare revenues. (Jackson Memorial
receives approximately 50 percent of state DSH payments.)
Jackson Memorial is the major safety net hospital in Dade County, account-
ing for 50 percent of all Medicaid inpatient days in the market in 1993 and 55
percent of all charity care and bad debt ($124 million in 1995).
48
Whether or not
there are other safety net hospitals is a subject of debate. While certain hospitals
provide significant amounts of care to Medicaid-eligible people, they provide
relatively little charity care compared with Jackson Memorial. These facts have
called into question the manner in which local, state, and federal funds are
distributed. The mayor’s office and the South Florida Hospital Association
argue that other hospitals in Dade County, which together provide about 50 per-
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
42

cent of the care to the low-income and uninsured population, should receive
some of the funds from the half-cent tax. The mayor’s office would like to
decentralize health care along lines similar to those in Hillsborough.
49
In the past few years, Jackson Memorial’s share of the Medicaid market has
declined because of increasing competition for Medicaid patients. According to
Jackson Memorial officials, between 1990 and 1995, Medicaid inpatient days
dropped from 484,000 to 391,000, a 20 percent decline. Whereas Jackson
Memorial once provided 90 percent of obstetrics care to low-income patients,
its share has dropped to 50 percent. A priority for Jackson Memorial has been to
maintain patients, primarily Medicaid patients, in its system. To do so, it has
expanded its primary care patient referral base; it now owns or affiliates with
six primary care clinics. It has also expanded an existing managed care plan
(Jackson Memorial Hospital Health Plan), which recently won a contract in
the Medicaid managed care bidding process. It created a new managed care
plan (with a private managed care plan and University of Miami Hospital) to
capture more of the Medicaid and commercial capitated market. In addition, it
is lobbying the state to modify the certificate-of-need regulations so that it can
convert hospital beds into swing beds. Finally, the hospital is attempting to
reduce costs through cuts of up to 1,000 full-time employees.
Nine primary care centers in Dade County provide care to low-income peo-
ple. The growth of Medicaid managed care has resulted in a loss of revenues for
all community clinics, creating substantial financial problems. In some cases,
clinics have lost Medicaid patients and the revenues that they provided, result-
ing in a loss of some capacity to subsidize care for the uninsured. In other cases,
clinics have lost Medicaid revenues but have continued providing care to
Medicaid patients assigned to other primary care providers and uninsured
patients, presumably with funds provided in their grants from the federal
Bureau of Primary Health Care. Some are reconsidering their mission in light
of these changes; while federal grants and FQHC cost-based reimbursement
have served as a cushion, some clinics believe they are at the end of their rope.
Community clinics in Dade County have pursued a variety of strategies to
maintain their competitiveness and Medicaid patient base. A group of four
major clinics banded together to form Health Choice Network to conduct joint
purchasing, integrate management information and fiscal systems, coordinate
medical directorships, and create market power to negotiate with managed care
plans. Health Choice has been fairly successful in negotiating contracts with
hospitals and health plans because of its large Medicaid obstetrics patient base.
It has referral relationships with several hospitals, but not with Jackson because
Jackson does not refer patients back to the clinics and does not offer admitting
privileges to Health Choice’s physicians. In addition, Jackson opposes having
the Trust, or any county funds, provide financial support to the clinics.
Like other county public health units, Dade County’s health department had
for many years provided both traditional public health services and compre-
hensive primary care services. Between 1993 and 1995, Medicaid encounters
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
THE URBAN
INSTITUTE
43

decreased by about 30 percent, causing the department to rethink its mission.
Seeing a rise in communicable diseases, such as AIDS and tuberculosis, the
county decided that it should not continue to provide primary care services. It
issued an RFP for an organization to take over its maternity and pediatrics ser-
vices in four clinics. Jackson Memorial’s bid was accepted in part because of
its assurance that it would maintain a commitment to providing care to the
uninsured, including documented and undocumented aliens. The county has
maintained two clinics, which provide family planning, immunizations, and
other traditional public health services.
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
44
Long-Term Care for the Elderly
and Persons with Disabilities
T
he need for long-term care services for older adults is potentially enor-
mous in Florida. In 1995, 2.7 million people, or 19 percent of the state’s
population, were over the age of 65, which is substantially higher than
the national average of 12.7 percent and makes Florida the state with
the greatest proportion of elderly. Given this, there is substantial pressure to
develop a larger, but low-cost, system of long-term care.
Supply, Expenditures, and Utilization
As in other states, long-term care in Florida is heavily financed by the
Medicaid program, and long-term care services are an important part of the total
Medicaid budget, though less than in many other states. For example, in 1995,
the state spent 28 percent of its total Medicaid budget on long-term care ser-
vices, compared with a national average of 34 percent. Medicaid spending on
long-term care in the state grew slightly more rapidly than other components
of the Medicaid program between 1992 and 1995, at an annual rate of 14.7 per-
cent, about twice the national rate (table 6). However, long-term care spending
per elderly and blind and disabled recipient was still 36 percent lower than
the national average in 1995, primarily because of a low supply of nursing-
home beds and relatively little spending on home and community-based care.
In 1996, there were 699 certified nursing homes and 79,000 long-term care
beds in Florida. Occupancy rates in Florida nursing homes are about 91 per-
cent. While the state’s certificate-of-need law allows the number of beds to rise
if the occupancy rate increases, Florida’s ratio of 30 beds per 1,000 people over
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
46
Table 6 Medicaid Long-Term Care Expenditures by Eligibility Group, Florida and United States (Expenditures in Millions)
Florida United States
Long-Term Care Average Annual Long-Term Care Average Annual
Expenditure Growth Expenditure Growth
1990 1992 1995 1990–92 1992–95 1990 1992 1995 1990–92 1992–95
Total $864.4 $1,173.4 $1,769.3 16.5% 14.7% $32,264.2 $42,542.5 $53,996.1 14.8% 8.3%
Elderly $579.2 $796.9 $1,117.5 17.3% 11.9% $18,408.9 $24,846.4 $30,413.7 16.2% 7.0%
Nursing Home Care 560.2 766.5 1,052.9 17.0% 11.2% 15,131.3 20,542.9 25,571.5 16.5% 7.6%
ICFs/MR
a
2.0 2.7 6.8 16.3% 36.0% 348.9 452.0 615.8 13.8% 10.9%
Mental Health 9.1 11.9 13.3 14.3% 3.8% 973.0 1,286.0 1,107.3 15.0% –4.9%
Home Care 7.9 15.8 44.5 41.2% 41.2% 1,955.7 2,565.6 3,119.1 14.5% 6.7%
Blind and Disabled $282.2 $363.8 $632.5 13.5% 20.3% $12,842.4 $16,201.0 $21,618.7 12.3% 10.1%
Nursing Home Care 87.2 117.1 157.0 15.9% 10.3% 3,161.3 3,968.0 4,813.3 12.0% 6.6%
ICFs/MR
a
155.1 179.0 239.8 7.4% 10.2% 7,241.3 8,380.4 9,321.1 7.6% 3.6%
Mental Health 0.8 1.4 1.4 30.4% –0.5% 457.9 682.1 881.3 22.1% 8.9%
Home Care 39.1 66.2 234.4 30.1% 52.4% 1,982.0 3,170.5 6,603.0 26.5% 27.7%
Adults and Children 2.9 12.8 19.2 108.2% 14.6% 1,012.9 1,495.1 1,963.7 21.5% 9.5%
Source: The Urban Institute, 1997. Based on HCFA 2082 and HCFA 64 data.
a. Intermediate care facilities for the mentally retarded.
age 65 was one of the lowest in the country in 1994, compared with a national
average of 53.3 per 1,000 elderly.
50
As of 1994, there were 1,450 licensed home
health care agencies in Florida. There were also 120 licensed adult day care
centers and 2,364 licensed residential care facilities in 1994, including assisted
living facilities and adult family-care homes.
51
Other types of facilities serve the developmentally disabled. These include
four state-operated Developmental Services Institutions. Most of the beds in
these facilities are certified as ICF/DD and serve approximately 15,500 indi-
viduals at any given time. In addition, there are 2,200 beds in privately operated
ICFs/DD and 804 long-term residential care facilities with 5,778 licensed beds.
In 1994, 44 percent of persons with developmental disabilities in institutional
settings were in facilities with more than 16 beds.
Long-Term Care for the Elderly
Florida spent $1.1 billion in 1995 on long-term care for the elderly (table 6).
The state relies more heavily on nursing home care to provide long-term care ser-
vices to the elderly than do most other states. In 1995, 94 percent of long-term
care expenditures for the elderly under the Medicaid program were for nursing
home services, compared with 84 percent nationally. Spending on nursing home
care for the elderly rose more rapidly than the national average, at an annual rate
of 11.2 percent between 1992 and 1995. (The national rate was 7.6 percent.)
While nursing home bed supply is allowed to increase, it is carefully regulated
by the state.
Reorganizing the Delivery System
Although there appears to be growing interest in expanding home and com-
munity-based care for the elderly and disabled, Florida continues to lag behind
most states in doing so. Advocates and policymakers acknowledge that the
current system of nursing home care, with its low number of beds, may be
unsustainable and that there is likely to be huge demand in the long run. Yet
policymakers remain concerned that offering home and community-based ser-
vices will be unaffordable. The nursing home industry supports alternatives to
nursing homes, including the small waiver programs the state has imple-
mented, because it believes that if the state purchases services more cost effec-
tively, it can stretch current long-term care dollars further.
Florida operates a state-funded long-term care program called Community
Care for the Elderly (CCE), which helps functionally impaired elderly live in the
least restrictive environment suitable to their needs. In FY 96–97, the state
will spend a projected $41 million in state general revenues to provide com-
munity-based services to approximately 38,500 functionally impaired older
people, including those served under a Medicaid home and community-based
services waiver.
52
All CCE clients are screened annually for Medicaid waiver
eligibility (see below); those found eligible and meeting level-of-care conditions
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
THE URBAN
INSTITUTE
47

are transferred to the waiver program, allowing the Department of Elder Affairs
to maximize federal funding. According to the Department of Elder Affairs,
another 8,000 to 11,000 are on the waiting list. Priority is given to those who are
at risk of entering an institution or those who have been abused, neglected, or
exploited.
The Department of Elder Affairs and AHCA share responsibility for admin-
istering the state’s several home and community-based care waivers that serve
the elderly. The primary home and community-based care waiver for the
elderly is a 1915(c) waiver that diverts disabled adults and elderly from nursing
facilities. Elderly individuals qualifying for Medicaid and assessed by a health
professional as frail, functionally impaired, and at risk of nursing home place-
ment are eligible for services under the waiver. The FY 96–97 estimated bud-
get for all services under this waiver was $36.1 million. The federally assigned
maximum enrollment cap in this waiver program for FY 96–97 is 16,943, but
only 9,550 individuals are expected to receive services under the program,
because the state has not appropriated the required matching funds.
53
While the nursing home bed supply in Florida is quite low, the state has
more licensed residential care beds per 1,000 elderly population than the rest of
the nation (24.2 beds, compared with 20.1). Residential care facilities include
both assisted living facilities and adult family-care homes.
54
Assisted living
facilities are residential options for the elderly and disabled that provide hous-
ing, meals, and supportive services. Currently, there are more than 1,800
assisted living facilities statewide, serving more than 60,000 residents (averag-
ing 33 residents each); another 600 adult family-care homes serve about 1,200
residents. Most residents cover the cost of their own care in these facilities,
but the state provides a subsidy for some low-income residents.
55
There is no
state certificate-of-need requirement for assisted living facilities. Thus, the state
cannot regulate their growth. According to the Florida Commission on Aging
with Dignity, occupancy rates range from 70 percent to 80 percent, suggesting
ample capacity.
Although Florida’s apparent dearth of nursing home beds relative to its
proportion of elderly citizens has raised concerns about access, nursing home
industry representatives speculate that assisted living facilities and adult fam-
ily-care homes may be serving as providers to those not able to secure a nurs-
ing home bed. They also speculate that the elderly in Florida may have more
financial resources than those in other states and less need for public support
for nursing home care.
Traditional Cost Containment Methods
Nursing homes receive Medicaid reimbursement according to an adjusted
cost-based methodology, with rates determined prospectively on a per diem
basis. They are not case-mix adjusted. Medicaid currently pays on average $92
per day, higher than the national average of about $83 per day. Annual target
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
48

limits on increases are very low; the state did not recognize cost increases
resulting from changes contained in the federal Omnibus Budget Reconciliation
Act of 1987, for example.
The state regularly cuts funds from institutional care line items in the
Medicaid budget. Over the past five years, Medicaid has absorbed over $1 bil-
lion in budget reductions, a substantial amount of which was in the area of
institutional provider payments. For example, modifications to nursing home
reimbursement policy in 1991 resulted in a $31 million cut, followed by a $20
million cut in FY 92–93, a $13 million cut in FY 95–96, and a $17 million cut
in FY 96–97. Despite these reductions, nursing homes have not filed any Boren
amendment lawsuits, largely because they believe such suits consume too
many resources and have not produced the desired results.
The nursing home industry has made Medicaid reimbursement a perennial
priority issue. According to the Florida Health Care Association, 80 percent of
nursing homes report that their costs are not covered by Medicaid. The indus-
try reports that “high Medicaid homes” (those with more than two-thirds
Medicaid patients) are almost four times as likely to be under conditional status
(those with identified problems) than “low Medicaid homes.” Several nursing
home chains have been in administrative hearings with AHCA over July 1996
rate reductions (rather than Boren suits, which are filed in federal court).
Industry representatives predict that as budget reductions for institutional long-
term care continue, the state will see an erosion in the quality of patient care.
Certificate-of-Need Restrictions
As mentioned earlier, Florida has one of the lowest nursing-home bed sup-
plies in the country. Nursing home bed growth is carefully regulated by the
state. The bed supply increases by about 1,800 to 2,400 beds each year, based on
allowable growth limits under the state’s certificate-of-need law. According to
AHCA officials, there are 8,000 more long-term care beds currently in the con-
struction pipeline (under previous certificate-of-need approvals).
Medicaid Eligibility for Nursing Home and Home Care Services
Florida’s medically needy program does not cover institutional services
(nursing homes, ICFs/DD, and state mental hospitals), preventing qualification
for Medicaid through spend-down on nursing home expenses.
Many Miami nursing homes were concerned about the impact of the welfare
reform law on their Medicaid residents who are legal aliens. The state, however,
elected to continue Medicaid eligibility for those who entered the country prior
to August 1996, ensuring that the Medicaid nursing home benefit is secure for
most people. The general sense in the industry is that influential Miami legis-
lators will support funding of legal immigrants in nursing homes who will still
not qualify for Medicaid, estimated at 2,000 to 3,000 people.
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
THE URBAN
INSTITUTE
49
Medicare Maximization
In 1996, the legislature required AHCA to ensure that home health care ben-
eficiaries exhaust all Medicare benefits before using Medicaid coverage. It also
required prior authorization for home health care.
Limits on Transfer of Assets and Estate Recovery
The leader of an advocacy group for low-income elderly has publicly com-
plained that approximately 5 percent to 10 percent of new Medicaid appli-
cants become eligible through “artificial impoverishment schemes.”
56
While
Florida has yet to address this problem, in FY 96–97, the AHCA planned to
expand its estate recovery efforts.
57
SB 886 allows the Department of Revenue to
share estate information with AHCA’s Medicaid Estate Recovery Program,
which may increase recovery rates.
Younger People with Disabilities
Responsibilities for younger persons with disabilities are spread across a
number of agencies, including the Developmental Services Program, Department
of Mental Health and Substance Abuse, and Children’s Medical Services within
the Department of Health. The overall strategy for providing services to this pop-
ulation has been to reduce the reliance on institutional settings and increase
community-based care. However, for the developmentally disabled and the men-
tally ill, the need for both institutional and community-based services outpaces
the supply of services and state resources to purchase such services.
Institutions and Community-Based Services for the Mentally Ill and
Developmentally Disabled
In the early 1990s, Florida explicitly sought to maximize federal revenues
for covering the developmentally disabled through its Medicaid home and com-
munity-based services waivers. According to officials in the Developmental
Services program, two main waivers are used by the state of Florida for disabled
nonelderly populations: a Developmental Services waiver that covers almost
11,000 individuals and a smaller Aged/Disabled Assisted Living waiver that
covers about 1,300 people. The state currently has approval from HCFA for
20,000 individuals in the Developmental Services waiver, and the state has
authorized funding for 11,000 individuals. Increased use of these waivers has
allowed the state to serve individuals in community settings at a lower cost
than serving them in institutions. The movement to serve this population in the
community is seen as advantageous to the clients as well. Finally, the shifting
of the financing of care from the state to the federal government has allowed the
state to serve more clients with the same amount of state resources.
58
Despite the greater reliance on community-based care, of the 28,000 persons
served by the Developmental Services program (including through waivers),
more than 9,000 have been identified as having unmet needs. More than 90 per-
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
50

cent of these individuals are eligible for home and community-based waiver
services. A similar situation exists for persons with mental illness. According to
the governor’s budget recommendations, only 32 percent of the need for men-
tal health services in the state is being met.
A number of recent lawsuits have tested the issue of whether long-term care
services for the disabled are entitlements. In Does v. Chiles, plaintiffs alleged
that the state’s policy of rationing ICF/DD services by limiting ICF/DD beds
and putting qualified persons on waiting lists violates federal law and that the
state is not providing services with “reasonable promptness.” In July 1996 the
courts ruled that the waiting lists violated the reasonable promptness require-
ment and ordered the state to address this in their Medicaid plan and limit
waiting list time to no more than 90 days. The state estimates that it would
cost $700 million to comply, and it has appealed the decision. This suit essen-
tially will determine whether ICF/DD services are an entitlement.
In the 1995–96 session, the legislature determined that ICF/DD services
(which are optional) are a “runaway cost item” and decided that the state would
no longer fund services in privately owned ICF/DD facilities. With the change
in legislation, the state also removed $34 million from the Developmental
Services program budget. In response, the Cramer v. Chiles suit was filed, with
plaintiffs contesting the legislation. The plaintiffs alleged that there was no plan
to transition the 2,200 individuals currently in privately owned ICFs/DD into
other programs, namely the home and community-based services waiver pro-
gram. The court granted a preliminary injunction that the state continue to pay
for 100 percent of the costs of those individuals currently in privately owned
ICFs/DD until the state completes a plan to transition these individuals into a
community-based setting approved by HCFA.
The outcomes of the state’s appeals of these two decisions will likely set
the tone for the provision of long term-care services for disabled persons over
the next few years.
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
THE URBAN
INSTITUTE
51
Challenges for
the Future
F
lorida faces a number of major challenges in the near future. A primary
concern is the size and scope of the Medicaid program. Governor Chiles
has proposed the expansion of Medicaid coverage for children under
age 3 with household incomes up to 185 percent of the federal poverty
level; he has also requested authorization to increase the number of children
covered by the Healthy Kids program to more than 100,000. However, growth in
Medicaid expenditures in the past decade has made the Medicaid program a
serious target for budget cutters interested in allocating more funds to education
and corrections. Reductions in Aid to Families with Dependent Children case-
loads and a number of other factors have mitigated the impact of these cuts on
the program in the past. However, any change in the rosy economic situation
in Florida could create problems, forcing state officials to make decisions
regarding the core of the Medicaid program: eligibility levels and benefits. At
the same time, over 19 percent of the state’s population lacks health insurance
of any kind, despite rapid growth in Medicaid enrollment in recent years. With
the passage of its State Child Health Insurance Program, the state is likely to
expand coverage further for children. But given recent cuts in the program,
Medicaid expansions to cover other uninsured populations are unlikely.
Moreover, the state faces a challenge with respect to both welfare reform and
long-term care. Welfare reform provisions will end Medicaid assistance to
future legal immigrants in Florida. Although some interest has been shown in
extending state-funded coverage to those individuals already in the United
States who were made ineligible for Medicaid, it will come at some cost to the
state. Failure of the state to act will mean costs to local areas.

Florida has the largest elderly population in the country, yet it currently
spends comparatively little on long-term care; demand for these services is
expected to rise considerably. The nursing home bed supply is low by national
standards, and the state has restricted increases in nursing home payment in
recent years, raising concerns about the impact on the quality of care. The state
is also under pressure to expand long-term care services at home and in the
community.
The state’s attempt to expand coverage through insurance reform has been
only partially successful. The state had hoped, with reform in the small group
market and the development of Community Health Purchasing Alliances
(CHPAs) to reduce the cost of health care and expand insurance coverage. To
date, there has been little downward pressure on premiums. Moreover, the
CHPAs have been only partially successful at expanding coverage to small
businesses, in part because of legislative constraints on their bargaining abil-
ity. Florida faces a challenge in making the CHPAs more efficient, as well as in
expanding insurance reform to the individual market.
In general, the Florida provider market is experiencing rapid change. The
state has experienced considerable growth in commercial managed care. At
the same time, Florida’s health care market is experiencing rapid growth in
for-profit health maintenance organizations (HMOs) and for-profit hospitals.
Further consolidation among both HMOs and hospitals can be expected. It is
unclear whether or not this will lead to improved efficiency in the marketplace
and lower health care costs, and if so whether or not the lower costs come at the
price of quality. Equally important, it is unclear whether nonprofit hospitals
faced with increasing competitive pressures will continue to be able to pro-
vide services to low-income populations.
Alongside the rapid growth in commercial managed care, the state has
embarked on a path of dramatic increase in the number of individuals in
Medicaid managed care, the results of which are uncertain. Enrollment abuses
and quality-of-care problems have led to calls for increased regulation of the
Medicaid managed care industry. In Florida as in other states, there are likely to
be a number of proposals for managed care regulation in the near term, which
could have important implications for Medicaid as well as for the nature of
market competition in the state.
With strong antitax sentiment throughout the state, prospects for expand-
ing the state role in health care financing are uncertain. (Enactment of the State
Child Health Insurance Program in August 1997, with the offer of substantial
new federal funds, will alter these prospects.) Safety net institutions, both hos-
pitals and community health centers, are facing serious competitive pressures.
They are finding it more difficult to compete for Medicaid patients because of
the increase in Medicaid managed care. The growth in Medicaid managed care,
coupled with the large uninsured rate, places a large burden on local providers
and on local governments. In Dade and Hillsborough Counties, local taxes have
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
54

been increased to fund a small insurance program (Hillsborough) and to sup-
port a major hospital (Dade). The safety net could be threatened if a recession
occurs or if the local areas are unable to sustain public support for these insti-
tutions and their mission. The state has increased its support of Tampa General
Hospital and may have to play a greater role in supporting the safety net
throughout Florida in the future.
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
THE URBAN
INSTITUTE
55

Notes
1. State of Florida, The Governor’s Budget Recommendations, FY 1997–98. Summary, January
1997.
2. State of Florida, The Governor’s Budget Recommendations, FY 1997–98, Summary, January
1997.
3. State of Florida, The Governor’s Budget Recommendations, FY 1997–98, Summary, January
1997.
4. Department of Children and Families, Impact of Restrictions on Legal Immigrants, February
1997.
5. Agency for Health Care Administration, Medicaid Statistics: Florida Medicaid Program,
November 30, 1996.
6. State of Florida, The Governor’s Budget Recommendations, FY 1997–98, Summary, January
1997.
7. Agency for Health Care Administration, Medicaid Statistics: Florida Medicaid Program,
November 30, 1996.
8. Eligibility is based on Medicaid criteria for children up to age 13; older children must be in
families earning under the federal poverty level. The program has 23 local offices and numer-
ous providers under contract who provide services to children with physical disabilities
that traditional providers may not be qualified to treat. Services are funded largely through
Medicaid revenues (72 percent to 73 percent), with federal Title V and some state funds
covering the costs of the uninsured.
9. Legislators Guide to Medicaid, 1997.
10. The Boren amendment required states to pay hospitals and nursing homes the costs associ-
ated with an economically and efficiently operated facility (that meets quality and safety
standards). The Boren amendment was repealed by the Balanced Budget Act of 1997.
11. State of Florida, The Governor’s Budget Recommendations, FY 1997–98, Summary, January
1997.
12. Urban Institute calculations based on HCFA 2082 data and projections from the March 1994
Current Population Survey, in “Medicaid Expenditures and Beneficiaries: National and State
Profiles and Trends: 1984-1994,” Kaiser Commission on the Future of Medicaid, November
1996, page 31.
13. Florida Agency for Health Care Administration, Medicaid Services Budget Forecasting
System Reports. These figures are less than the number of enrollees in 1995 reported in the
Urban Institute’s analysis of HFCA 2082 data, which counts all of those enrolled at any time
during the year.
14. For further details, see Ku, Leighton, “Florida Health Security Program,” in Increasing
Insurance Coverage through Medicaid Waiver Programs: Case Studies, Urban Institute,
November 1994, pages 79–93.
15. Healthy Kids, 1997 Annual Report, February update.
16. Healthy Kids, 1997 Annual Report, February update.
17. These counties are Alachua, Broward, Collier, Dade, Duval, Escambia, Flagler, Hardee,
Hendry, Highlands, Hillsborough, Okeechobee, Palm Beach, Pinellas, St. Lucie, Santa Rosa,
and Volusia. Another 12 counties have been designated as planning sites, and 3 counties are
designed as future sites.
18. The Florida Comprehensive Health Association is the state’s high-risk pool, which was
designed to cover individuals whose prior medical conditions made it difficult for them
to obtain coverage. It caps premiums at 200 percent to 300 percent of the standard low-
risk individual rate and is funded through enrollee premiums and assessments on insur-
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
THE URBAN
INSTITUTE
57

ance carriers. There are currently 2,387 enrollees, but enrollment was closed in July 1991
to new enrollees because insurers did not want to pay for anticipated losses. If the pool
were reopened, one possible source of funding would be an assessment on health care
providers.
19. Office of Health Policy, AHCA, Request for Proposals: Health Care Practice in a Reformed
Market, June 1995.
20. Community Health Purchasing Alliance, Monthly Program Report.
21. Office of Program Policy Analysis and Government Accountability, Review of the Status of
Community Health Purchasing Alliances in Florida, Report No. 96-5, September 1996.
22. Florida Hospital Association, FHA Eye on the Market: Health Care in the Sunshine State,
1996.
23. Department of Insurance, Annual Ranking Report of Licensed HMOs in the State of Florida,
December 31, 1995.
24. FAHMO members are largely commercial HMOs. FAHMO does not include some licensed
plans that have chosen not to join, nor does it include several HMOs that primarily enroll
Medicaid clients, which created their own association. The two groups sometimes split on
issues related to managed care.
25. Many of these bills did pass the legislature, but at the time of this report, were awaiting action
by the governor. See HB 297 and HB 325—Managed Health Care Entities, SB 244—Direct
Access to Dermatologists. An update can be obtained on the World Wide Web:
http://www.leg.state.fl.us/senate/summary/health.html.
26. Florida Hospital Association, FHA Eye on the Market: Health Care in the Sunshine State,
1996.
27. Florida Hospital Association, FHA Eye on the Market: Health Care in the Sunshine State,
1996.
28. One interviewee indicated that current Medicaid payments represented only 72 percent of
costs. The reason for the discrepancy in measures of generosity may be a function of varia-
tions in period, different data sources, or a hospital-specific issue.
29. Agency for Health Care Administration, Medicaid Services: Summary of Disproportionate
Share Hospital Payments, Fiscal Years 1987–88 through 1996–97.
30. According to FY 96–97 state budget documents, intergovernmental transfers account for only
$72.4 million of DSH revenues. The reason for the decline is not clear.
31. Norton, Steve, “Medicaid Fees and the Medicare Fee Schedule: An Update,” Health Care
Financing Review, vol. 17, no. 1, pp. 167–87.
32. State of Florida, The Governor’s Budget Recommendations, FY 1997–98, Summary, January
1997.
33. A study by Florida State University showed that MediPass saved 13 percent over traditional
FFS. Barrilleaux, C. et al., “Florida MediPass Evaluation Report,” submitted to Florida
Agency for Health Care Administration, December 1995.
34. Information from various sources: Agency for Health Care Administration. Medicaid
Statistics. Florida Medicaid Program. November 30, 1996. Legislators Guide to Medicaid.
Health Care Financing Administration Managed Care Report, 1995 and 1996.
35. SB 886 specified that new assignees who had not made a choice between MediPass or a
Medicaid HMO would be equally distributed between the two programs and allowed them 90
days to make a choice. However, the “Cut Bill” changed this to a 30-day period and required
that in the first quarter 60 percent of enrollees who have not made a voluntary choice be
assigned to Medicaid HMOs and 40 percent be assigned to MediPass. AHCA’s plan is to look
at the actual ratio of voluntary preference for four quarters and revisit the assignment ratio
at that point.
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
58

36. A separate Section 1115 waiver request is being prepared that would allow the state to lock
Medicaid recipients into either an HMO/PHP or MediPass for a period of one year, after a
Medicaid recipient has been given 30 days to make a choice and 60 days to switch plans.
37. In April 1995, the state lifted enrollment caps for eight Medicaid HMOs that were found to
meet 90 percent to 98 percent of all 46 contract standards. Those meeting less than 90 percent
of quality standards were subject to fines and penalties, enrollment caps at previous levels,
or a halt on expansion into other counties.
38. Until recently, only $1 million was available for enrollee education; this was just enough to
print brochures and operate a hotline (which opened in November 1996).
39. The RFP was issued at the end of August 1996, with a submittal deadline of October 4, 1996.
The RFP called for posting notices of intent to award on December 2 and awarding contracts
by January 1, 1997. But the process was held up for a couple of months by a protest against
the RFP, filed by one of the major Medicaid HMOs. A settlement was reached that allowed the
process to continue, and the notice of intent to award was issued on February 12, 1997.
However, as of mid-April, contracts had still not been signed, again due to some protests.
40. Agency for Health Care Administration, 1996–97 Medicaid Prepaid Health Plan: Model
Contract.
41. A bill passed by the legislature in 1997, but not yet signed by the governor, would extend
from July 1, 1997, to January 1, 1998, the time period for FQHCs and county plan providers
that contract with Medicaid as prepaid plan providers to be licensed by the Department of
Insurance as HMOs. It also prohibits the FQHCs from receiving prepaid reimbursement dur-
ing this interim period.
42. “Nationally Honored Health Care Plan Rates County Legislators’ Strong Support,” editorial,
Tampa Tribune, 1/10/97.
43. Undocumented aliens are not eligible for the program.
44. Hillsborough County, Hillsborough County Health Care, 1997.
45. On May 1, 1997, it was reported that the Florida legislature passed a bill on April 29 allow-
ing Hillsborough County “to continue collecting a sales tax to pay for its health plan for
the poor,” according to the Tampa Tribune. The bill, “now certain to win approval from Gov.
Lawton Chiles (D),” represents a compromise in which the county’s half-cent sales tax
would be extended until 2005, but the county commission “is expected to cut the tax in
half for four years to spend down part of a $114 million surplus.” The measure would also
allow the county “to roll back” its $26.8 million property tax to support the program. This
turn of events is likely to mean no expansion in the program, and it may even have to cut
back somewhat.
46. Agency for Health Care Administration, Medicaid Services: Summary of Disproportionate
Share Hospital Payments, FY 1995–96.
47. Florida Hospital Association, FHA Eye on the Market: Health Care in the Sunshine State,
1996.
48. Agency for Health Care Administration Hospital Financial Data, 1995. American Hospital
Association Annual Hospital Survey Data, 1993.
49. On January 16, 1992, then–County Commissioner Alexander Penelas published Health Net,
a report that described a decentralized indigent care program modeled after the Hillsborough
plan. No new plan has been developed, but respondents indicated that this plan was still
considered a plausible option.
50. American Association of Retired Persons, Across the States, 1996.
51. American Association of Retired Persons, Across the States, 1996.
52. Florida Department of Elder Affairs, Resource Manual, 1997.
53. Florida Department of Elder Affairs, Resource Manual, 1997.
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
THE URBAN
INSTITUTE
59
54. American Association of Retired Persons, Across the States, 1996.
55. Florida Department of Elder Affairs, Resource Manual, 1997.
56. H. James Towey, “Millionaires on Medicaid,” commentary in St. Petersburg Times, December
8, 1996.
57. Legislators Guide to Medicaid, 1997.
58. Department of Health and Rehabilitative Services, Monthly Data Report, September 1996.
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
60
APPENDIX
List of People
Interviewed
TALLAHASSEE
State Government
Agency for Health Care Administration
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
THE URBAN
INSTITUTE
61
Department of Children and Families
John Bryant
Susan Dickerson
Department of Elder Affairs
Charlie Liem
Department of Health
Donna Barber
James Howell, M.D.
Rick Hunter, M.D.
Department of Insurance
Michele Newell
Tom Warring
Office of the Governor, Planning and Budgeting Office
Paul Belcher
State Legislators and Legislative Staff
Representative George Albright
Lynn Dixon
Michael Hansen
John Wilson
Provider/Plan Associations
William Bell Florida Hospital Association
Greg Glass Florida Primary Health Care Association
Erwin Bodo Florida Health Care Association (nursing homes)
Richard Dorff Florida Association of HMOs
Tom Arnold
Doug Cook
Marilyn Y. Evert
Kate Morgan
Sally Morton
Nancy Ross
Bob Sharpe
Dyke Snipes
Celeste Putnam-Tanzy

Advocacy Groups
Marcia Beach Advocacy Center for Persons with Disabilities
Jack Levine Florida Center for Children and Youth
James Towey Florida Commission on Aging with Dignity
Others
Rose Naff Florida Healthy Kids Corp.
TAMPA/HILLSBOROUGH COUNTY
Hospitals
David Rogoff St. Joseph’s Hospital
Bruce Siegel, M.D. Tampa General Hospital
Community Health Centers
Burt Parmer Suncoast Community Health Centers, Inc.
Gloria Elliott Tampa Community Health Centers
Terrence Shirley Tampa Community Health Centers
City/County Officials
Phyllis Busansky Former County Commissioner
Douglas Holt Hillsborough County Department of Health and
Social Services
Cretta Johnson Hillsborough County Department of Health and
Social Services
Victor Martinez, M.D. Hillsborough County Department of Health and
Social Services
Pat Bean Deputy County Administrator
Others
Cynthia Sampson Community Health Purchasing Alliance District 6
Charles Mahan University of South Florida School of Public Health
Jay Wolfson University of South Florida School of Public Health
MIAMI/DADE COUNTY
Hospitals
Joseph Rogers Jackson Memorial Hospital
Harold Rohrer Jackson Memorial Hospital
Sandy Sears Jackson Memorial Hospital
Cliff Bauer Hialeah Hospital
Linda Quick South Florida Hospital Association
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
62

Community Health Centers
Stanley P. Balsley Stanley C. Myers Community Health Center, Inc.
Betsy Cooke Health Choice Network
Beverly Press Stanley C. Myers Community Health Center, Inc.
Fatima Zafar, M.D. Economic Opportunity Family Health Center
City/County Officials
Lillian Rivera Dade County Public Health Department
Joseph Romallo Dade County, Office of the Mayor
Others
Modesto Abety Dade County Children’s Services Council
Jenni Bergal Fort Lauderdale Sun Sentinel
Gary Clarke PCA Family Health Plan
Fred Schulte Fort Lauderdale Sun Sentinel
HEALTH POLICY FOR LOW-INCOME PEOPLE IN FLORIDA
THE URBAN
INSTITUTE
63
About the Authors
Debra J. Lipson, currently a health policy consultant in Geneva, Switzer-
land, at the World Health Organization, continues her work on projects related
to safety net providers. She was formerly associate director of the Alpha Center,
where she managed research studies on state and local health care reform, with
an emphasis on the financing and organization of health services for the poor
and uninsured.
Stephen Norton is a research associate at the Urban Institute’s Health Policy
Center, where he specializes in research on the Medicaid program, maternal
and child health, and those institutions providing care to the medically indi-
gent. He is the author of a number of articles on health care. Most recently, his
work has focused on assessing the impact of the Medicaid expansions to preg-
nant women and children on access to care, the displacement of private insur-
ance, and provider uncompensated care burdens.
Lisa Dubay is a senior research associate in the Urban Institute’s Health
Policy Center. Ms. Dubay’s recent research has focused on the impacts of
Medicaid expansions for pregnant women and children on health outcomes
and insurance coverage. In other work, she is assessing the impacts of Medicaid
managed care on access to care and birth outcomes for pregnant women, and
the extent to which defensive medicine operates in obstetrics. Ms Dubay has
published numerous articles in health policy journals.
Errata
Several published State Reports and Highlights include an error in Table 1, “State
Characteristics.” Incorrect figures were included for noncitizen immigrants as a
percentage of the population. Corrections were made on August 13, 1998 to both the
HTML and PDF version of these reports on the Assessing New Federalism website.
Correct figures for 1996
Noncitizens as a
Percent of the
Population
UNITED STATES 6.4%
Alabama 0.9%
California 18.8%
Colorado 5.1%
Florida 10.0%
Massachusetts 5.4%
Michigan 2.3%
Minnesota 3.0%
Mississippi 0.9%
New Jersey 8.8%
New York 11.9%
Oklahoma 1.5%
Texas 8.6%
Washington 4.3%
Wisconsin 2.1%
Source: Three-year average of the Current Population Survey (CPS) (March 1996-March 1998,
where 1996 is the center year) edited by the Urban Institute to correct misreporting of citizenship.
The error appears in the following publications:
State Reports:
Health Policy: Alabama, Colorado, Florida, Massachusetts, Michigan, Minnesota, Mississippi,
New Jersey, New York, Texas, Washington
Income Support and Social Services: Alabama, California, Massachusetts, Michigan, Minnesota,
Texas, Washington
Highlights:
Health Policy: Alabama, Florida, Massachusetts, Michigan, Minnesota, Mississippi, New
Jersey, New York, Oklahoma, Texas, Washington
Income Support and Social Services: Minnesota, Texas

The Urban
Institute
Phone: 202.833.7200
Fax: 202.429.0687
E-Mail: [email protected]
http://www.urban.org
State Reports
2100 M Street, N.W.
Washington, D.C. 20037
Nonprofit Org.
U.S. Postage
PAID
Permit No. 8098
Washington, D.C.
