March 2018
This report was prepared by the
Trust for America’s Health, with funding from
The John A. Harord Foundaon
Challenges, Opportunities,
and
Next Steps
Creating an Age-Friendly
Public Health System

P a g e 1 | 18
Creating an Age-Friendly Public Health System:
Challenges, Opportunities, and Next Steps
Amanda J. Lehning and Anne De Biasi
Table of Contents
Executive Summary 2
Aging and Public Health 3
Demographic Changes and an Aging Society 4
Challenges and Opportunities of an Aging Society 5
An Age-Friendly Paradigm Shift 6
A Framework for an Age-Friendly Public Health System 7
Barriers to C reating an Age-Friendly Public Health System 11
Next Steps 12
Participant List 14
Endnotes 16
Amanda J. Lehning is an assistant professor at the University of Maryland, Baltimore School of Social Work and a former
Health and Aging Policy Fellow with the Office of the Surge on General. Her research focuses on progra ms, polic ie s, and
neighborhood infrastructure that pr omote the optimal health, well-being, and ability to age in place of older adults.
Anne De Biasi is director of policy develop ment at the Trust for America’s Health (TFAH). She is responsible for defining
the agenda and strategy associated with TFAH’s goal to create a modernized, acco untable public health system and to
integrate preventio
n into a re forming health care system.
Trust for America’s Health is a nonprofit, nonpartisan o rganization d edicated to saving lives by protecting the health of every
community and working to make disease prevention a national priority.
The John A. Hartford Foundation is a national philanthropy dedicated to improving the care of older ad ults.
The Milbank Memorial Fund is a n e ndowed operating foundation that works to improve the health of populations by
connecting leaders and decision makers with the best available evidence and experience
.
Page 2 | 18
Executive Summary
Trust for America’s Health (TFAH), funded by The John A. Hartford Foundation, held a convening
called A Public Health Framework to Support the Improvement of the Health and Well-being of Older
Adults, in Tampa, Florida on October 27, 2017. National, state, and local public health officials; aging
experts, advocates, and service providers; and health care officials came together to discuss how public
health could contribute to an age-friendly society and improve the health and well-being of older
Americans. The goal of the convening was to develop a public health framework to support the
improvement of the health and well-being of older adults, focusing on areas where public health can
support, complement, or enhance aging services. Secondary goals included learning from the innovative
aging work in Florida and building rapport between the public health and aging sectors.
Participants strongly endorsed a greater role for public health in supporting the improved health and
well-being of older adults. The convening process began with presentations and discussions designed to
build a shared understanding of the strengths and challenges of both the aging services and public health
sectors. Through an examination of case studies of older adults, participants identified gaps in services,
supports, and policies needed to improve the health and well-being of older adults, and considered the
potential roles public health could play in filling these identified gaps. The convening resulted in a
preliminary Framework for an Age-Friendly Public Health System, described below, that outlines the
functions that public health could fulfill, in collaboration with aging services, to address the challenges
and opportunities of an aging society. The main takeaway from the convening was the need for an age-
friendly public health system that recognizes aging as a core public health issue.
For the purposes of the convening and this summary report, supporting healthy aging is defined as
comprising three key components: 1) promoting health, preventing injury, and managing chronic
conditions; 2) optimizing physical, cognitive, and mental health; and 3) facilitating social engagement.
i
This definition intentionally does not equate healthy aging with the absence of disease and disability.
Instead, it portrays healthy aging as both an adaptive process in response to the challenges that can occur
as we age and a proactive process to reduce the likelihood, intensity, or impact of future challenges.
Healthy aging involves maximizing physical, mental, emotional, and social well-being, while
recognizing that aging often is accompanied by chronic illnesses and functional limitations, including
lifelong conditions. And it emphasizes the importance of meaningful involvement of older adults with
others, such as friends, family members, neighbors, organizations, and the wider community. While the
public health sector has experience and skill in addressing these components of health for some
populations, it has not traditionally focused such attention on older adults.
The Framework for an Age-Friendly Public Health System developed at the convening includes five key
potential roles for public health.
1. Connecting and convening multiple sectors and professions that provide the supports, services,
and infrastructure to promote healthy aging.
2. Coordinating existing supports and services to avoid duplication of efforts, identify gaps, and
increase access to services and supports.
Page 3 | 18
3. Collecting data to assess community health status (including inequities) and aging population
needs to inform the development of interventions.
4. Conducting, communicating, and disseminating research findings and best practices to
support healthy aging.
5. Complementing and supplementing existing supports and services, particularly in terms of
integrating clinical and population health approaches.
This Framework should not be interpreted as a prescriptive guide to action or a declaration of the public
health sector’s oversight of such activities. Not every community will need public health to assume each
of these roles. In numerous instances, other organizations may already be actively engaged in such work
and the public health sector’s contributions may be unnecessary, limited, or primarily in support of the
efforts of others. The participants emphasized the importance of the many organizations and sectors
outside of public health with long and dedicated histories of providing services to older adults and
supporting healthy aging. The advancement of the public health sector’s work in this arena needs to be
guided by, and in partnership with, such organizations. Furthermore, public health organizations likely
will lack the sufficient resources to engage in all such activities and will need to carefully and
thoughtfully determine how and where to focus their energies. Nonetheless the convening participants
believed that the Framework offered a useful articulation of the potential contributions that the sector
should consider as it embraces a larger role in optimizing the health of older adults.
Aging and Public Health
There is a growing momentum for public health to contribute to programs, policies, and innovative
interventions to promote health and well-being for people as they age. While public health efforts are
partly responsible for the dramatic increases in longevity over the twentieth century,
ii
historically there
have been limited collaborations across the public health and aging fields. Older adults were not central
to the public health agenda when public health emerged in cities in the 19th century.
iii
Similarly, in the
mid-20th century, many federal and state policies to assist older adults to remain independent in the
community, including Medicare, Medicaid, and the Older Americans Act, did not explicitly call for a
role for public health organizations. Over the past 50 years, there have been some steps towards a more
collaborative approach, such as the formation of the Aging and Public Health section of the American
Public Health Association in 1978, or the mandated role for the Centers for Disease Control and
Prevention (CDC) in providing disease prevention and health promotion services offered through the
Older Americans Act in 1987.
iv
However, it is rare when local, state or federal public health agencies
have dedicated funding or develop initiatives targeting adults ages 65 and over.
In recent decades, the aging network, comprised of 56 State Units on Aging (SUAs), 655 Area Agencies
on Aging (AAAs), 243 Indian Tribal and Native Hawaiian Organizations, and thousands of service
providers and volunteers, has increasingly focused on prevention and wellness. The 2010 passage of the
Affordable Care Act (ACA) is shifting the health care system to one with a broadened focus on
prevention, wellness, and health, rather than only disease and injury. As mandated by the ACA, in 2011,
the National Prevention Council released the National Prevention Strategy with an overarching goal of
increasing the number of Americans who are healthy at every stage of life. In 2016, the Council
produced Healthy Aging in Action, which highlights current programs that are advancing the National
Page 4 | 18
Prevention Strategy specifically for older adults. Central to this report is the need for multi-sector
collaborations to achieve a goal of healthy aging.
Public health needs to be a critical partner in these efforts. Over the 20th century, public health played a
crucial role in adding years to life. In the 21st century, public health can play a crucial role in adding life
to years.
Demographic Changes and an Aging Society
Demographic changes make it critical for all sectors and professions, including those that have not
traditionally focused on older adults, to consider the needs of our aging society. In 1900, about three
million Americans, representing 4% of the total population, were ages 65 and over. By 2014, that
number had risen to 46 million, around 15% of the U.S. population. The oldest members of the baby
boom generation turned 65 in 2011, commencing a rapid increase in the number of older adults that will
continue until at least 2030. By that time, about one in five Americans will be 65 or older for the
foreseeable future.
v
This rise in the number and proportion of older adults only presents part of the picture, as there are
substantial variations within the older adult population. An increasing diversity along health and
sociodemographic dimensions means that policies and programs designed to meet the needs of older
adults must consider the needs and preferences of different subpopulations.
First, while the term “older adults” often refers to anyone over the age of 65 (or 60 for some programs),
there are differences in health and service needs between younger older adults and the “oldest old,”
comprised of those ages 85 and older. For example, while about one in eight people age 65 and older has
been diagnosed with Alzheimer’s disease, almost half of the oldest old has this disease.
vi
The 85 and
older population is projected to grow from six million in 2014 to 20 million by 2060.
vii
Second, the demographic composition of the older adult population is rapidly changing. For example,
the older adult population, much like the rest of the US population, is becoming more racially and
ethnically diverse. In 2014, 78% of older adults were non-Hispanic White, 9% were African American,
8% were Hispanic of any race, and 4% were Asian. By 2060, the percentage of non-Hispanic whites is
expected to drop to 55%, while the proportion of other racial groups will increase, with 22% of the
population Hispanic, 12% African American, and 9% Asian.
viii
These changes are important because of
racial and ethnic inequities in health and access to resources, as well as cultural differences in
expectations of informal and formal care.
Third, there are substantial variations in social and economic well-being among the older adult
population. Older adults are less likely to live below the poverty line than other age groups, with 10% of
those age 65 and over living in poverty in 2014,
ix
but this may not be an accurate indicator of economic
vulnerability in later life. Poverty increases with age, suggesting that the growth of the oldest old may
also lead to an increase in the number of older adults living in poverty. Additionally, because the federal
poverty line fails to take into account all of older adults’ basic living costs, including those for health
care and transportation, this measure underestimates the extent of financial need among this segment of
the population. Indeed, research using a more age-specific measure of financial resources found that in
Page 5 | 18
California more than half of older adults living alone and more than one-quarter of older couples lack
adequate income to cover basic expenses.
x
Challenges and Opportunities of an Aging Society
Existing systems and structures in the United States face major challenges in promoting the health and
wellbeing of this growing and increasingly diverse older adult population.
First, the United States lacks an overall system of long-term care, offering instead an uncoordinated and
often confusing patchwork of community-based programs with varying eligibility criteria, costs, and
availability. Long-term care is expensive for older adults, their families, and society. In the most recent
estimates available, spending on long-term services and supports (LTSS) totaled nearly $220 billion in
2012,
xi
a figure that may quadruple by 2050.
xii
Even with these high costs, LTSS are unable to fully
meet older adults’ needs. For example, 58% of those dually eligible for Medicare and Medicaid, a
population that often experiences health problems and disability, indicate they have unmet needs for
care for activities of daily living.
xiii
Second, family members and other informal caregivers are the largest sources of support for older adults
in this country, but changes in family structure and social roles limit the ability of family members to
provide that support. Decreased fertility rates, greater numbers of women in the workforce, and the
geographic dispersion of families have reduced the availability of younger family members to help older
adults with their daily activities.
xiv
While in 2013, there were more than 14 adults of prime caregiving
age (i.e., ages 45-64) for every person over the age of 85, by 2050, this ratio will drop to less than four
to one.
xv
If these trends continue, older adults may have fewer sources of instrumental assistance,
emotional support, and social interaction in the future.
Third, the physical and social infrastructures of many cities and towns in the United States create
barriers to healthy aging. For example, few older adults live in mixed-use neighborhoods where they can
safely walk to a grocery store, pharmacy, or other services and gathering places, and about one-third of
older adults do not have any public transportation where they live.
xvi
In addition, many places lack social
features that could help older adults remain connected to their community, such as adult learning
programs, volunteer activities that utilize their skills and experience, and other enjoyable and
meaningful activities.
While these challenges need to be addressed, the aging of the US population is also creating
opportunities for older adults and their families and communities. Too often, the changing demographics
of the United States are equated to a crisis, reflected in the use of the term “silver tsunami,” rather than
as a success story of improved health, well-being, and longevity. Today’s older adults, on average, have
higher educational attainment, better overall health, and lower disability rates than previous
generations.
xvii
Older adults serve their communities formally by engaging in volunteer activities, such
as tutoring in an elementary school, maintaining a community garden, registering residents to vote, and
working at a food bank, among others. Older adults also make valuable contributions through informal
roles. For example, 19% of all of those who provide care to an adult with health or functional limitations
are age 65 or older
xviii
and 2.7 million older adults are the primary caretakers of their grandchildren.
xix
Page 6 | 18
An Age-Friendly Paradigm Shift
In response to the challenges and opportunities of our aging society, in recent decades, there has been a
growing emphasis on making existing systems and structures more “age-friendly.” This approach
acknowledges the importance of assessing the fit between individual needs and preferences with their
surrounding environment.
One prominent example is the movement to create more age-friendly communities, defined as those that
encourage “active aging by optimizing opportunities for health, participation, and security in order to
enhance quality of life as people age.”
xx
Age-friendly community initiatives typically focus on
modifying the physical and social infrastructure to support older adults’ health, well-being, and ability to
age in place. Age-friendly community features typically include two types of programs, policies, and
infrastructure: 1) those that focus specifically on the needs of older adults, and 2) those that benefit older
adults as well as community residents at other stages of the life course.
xxi
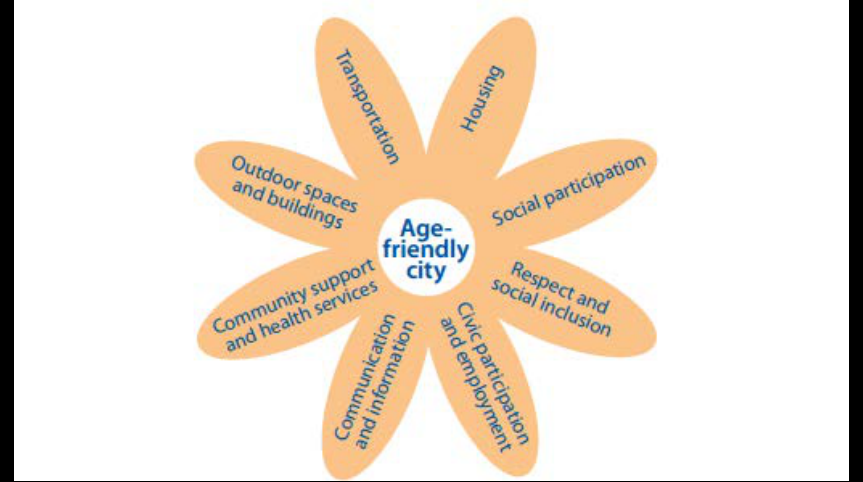
For example, the World Health
Organization’s Global Network for Age-Friendly Cities and Communities program
xxii
began in 2006 in
33 cities in 22 countries and now has more than 287 members (including US affiliates through the
AARP Network of Age-Friendly Communities). Based on information gathered from the scholarly
literature and more than 150 focus groups with older adults, caregivers, and service providers around the
world, the World Health Organization (WHO) identified eight core community features for an age-
friendly community (see Figure 1 on page 7). These features include those under the purview of public
and private sectors, as well as multiple disciplines and professions.
Figure 1: WHO Age-Friendly Community Features
Source: WHO global network for age-friendly cities and communities. (2014). Retrieved from:
http://www.who.int/ageing/age_friendly_cities_network/en
Page 7 | 18
There has also been movement toward the development of age-friendly health systems, spurred not only
by the projected increase in demand for health care as the proportion of older adults rises, but also by
innovations in health care delivery post implementation of the ACA, such as person-centered care,
bundled payments, and innovations addressing the social determinants of health.
xxiii
Age-friendly health
systems aim to provide evidence-based care via a trained geriatric workforce, coordinate with a full
range of community-based services, and meaningfully engage older adults and their families. The John
A. Hartford Foundation, for example, has made the expansion and evaluation of an age-friendly health
system approach a major priority, with the ultimate goal of developing effective strategies to improve
health outcomes and reduce costs.
An age-friendly public health system aligns with and complements these existing age-friendly
initiatives. It identifies the key capacities that public health potentially can bring to support ongoing
efforts by the aging and health care fields. It also highlights the ways public health expertise can inform
the development and implementation of new policy and programmatic interventions.
A Framework for an Age-Friendly Public Health System
The Framework for an Age-Friendly Public Health System identifies five key potential roles for public
health, with particular attention to the ways public health can support, complement, or enhance aging
services.
1. Connecting and convening multiple sectors and professions that provide the supports, services,
and infrastructure to promote healthy aging.
Addressing the full range of individual and community needs to support healthy aging requires the
active contribution of a variety of stakeholders. Many different organizations and professionals are
already working to support healthy aging, yet they often operate in silos with limited opportunities to
communicate with each other. The first potential role of public health is to connect and convene the
multiple sectors and professions that provide the supports, services, and infrastructure to promote
healthy aging.
One example that highlights this role is in promoting and supporting physical activity. Regular physical
activity reduces the risk of chronic conditions, such as diabetes and cardiovascular disease, prevents
cognitive and functional decline, and decreases the likelihood of falls and subsequent injury,
xxiv
however
only a minority of older adults meets recommendations such as the 2008 Physical Activity Guidelines
for Americans.
xxv
There are numerous barriers to regular physical activity in later life, including
restricted access to indoor and outdoor recreational facilities, concerns about neighborhood safety,
limited individual knowledge about the benefits of exercise,
xxvi
and the absence of walkable
neighborhood features (e.g., well-maintained sidewalks, raised crosswalks, speed bumps, and a variety
of food and shopping destinations).
xxvii
Public health could bring together the multiple actors that could
alleviate these barriers, including law enforcement, public works, parks and recreation, city planning,
local businesses, physicians, senior centers, and other community groups. As a connector and convener,
public health can promote communication across sectors and facilitate the sharing of knowledge and
resources.
Page 8 | 18
Another example is the need to address social isolation in later life. Social isolation can involve an
objective separation from a social network, such as living alone, or more subjective feelings of
loneliness.
xxviii
Approximately 12 million adults over the ages of 65 live alone,
xxix
and studies report that
15% to 45% of older adults experience loneliness.
xxx,
xxxiixxxi,
Social isolation can negatively affect
quality of life and contribute to an increased risk of morbidity and mortality.
xxxiii,
xxxiv
Public health can
work with community-based organizations, such as senior centers, community centers, and YMCAs, to
address loneliness and social isolation by providing opportunities for social interaction and the
development of new friendships. Public health professionals can also partner with “Villages,” grassroots
consumer-driven community-based organizations that aim to promote aging in place by combining
services, participant engagement, and peer support. First emerging in the early 2000s, currently there are
more than 200 Villages in the United States in operation or development.
xxxv
Studies suggest that
Villages are a promising approach to increasing members’ social engagement,
xxxvi
and connecting with a
variety of formal and informal community supports (including those offered by public health
departments) plays a critical role in their ability to do so.
When convening sectors, professions, and organizations, public health typically leverages its seat at the
table to ensure a focus on prevention and on policy, systems, and environmental change to support the
goals of healthy aging efforts. A greater focus on prevention can help forestall declines in health and
well-being, such as falls prevention and initiatives to promote physical activity or brain health. A focus
on policy, systems, and environmental change complements the efforts to address the needs of
individual older adults by focusing on improvements that impact entire populations or communities.
2. Coordinating existing supports and services to avoid duplication of efforts, identify gaps, and
increase access to services and supports.
Navigating the wide variety of supports and services for older adults can be confusing and
overwhelming for older adults, their families, and other professionals. Supports and services are offered
by a range of providers in different locations and settings, with different funding sources and variations
in eligibility requirements. A second critical role for public health is therefore to coordinate existing
supports and services to avoid duplication of efforts, identify gaps, and increase access to services and
supports. If there are available resources, health departments can create an aging specialist role to
facilitate this coordination and ensure that older adults are not overlooked in any other public health
programming or research.
It should be noted that aging professionals and organizations, including AAAs, are working to avoid
duplication of efforts, reduce unmet need for supports, and maximize the efficient use of existing
resources. Public health can be a particularly effective coordinator to address the barriers within its areas
of expertise. For example, many older adults do not receive preventive health services, such as those
recommended by the U.S. Preventive Services Task Force, including screenings, behavioral health
monitoring and counseling, and immunizations.
xxxvii
With 90% of flu-related deaths occurring among
those ages 65 and over,
xxxviii
there is a critical need to improve the availability and acceptability of such
preventive services. Public health has been a key partner in the work of Vote & Vax, a national initiative
that has received support from the CDC and the Robert Wood Johnson Foundation to provide flu
vaccines in polling places. Bringing together multiple sectors, including public health, pharmacy, and
nursing, Vote & Vax has demonstrated success in improving vaccination rates among those with access
barriers to the more traditional vaccination sites of physician offices or pharmacies.
xxxix
This program
Page 9 | 18
thus fills a critical gap in service delivery and highlights a creative approach to improving population
health.
3. Collecting data to assess community health status (including inequities) and aging population
needs to inform the development of interventions.
All sectors are becoming increasingly data driven to ensure that they have all the information they need
to address their target populations and target problems. A third role for public health is to call attention
to the needs and assets of a community’s aging population to inform the development of interventions
through community-wide assessment, a critical step to set goals and define measures for health
improvement.
Public health can help document population and community health status by collecting and analyzing
data, including data from multiple sectors and sources. While public health has often not focused on
older adults in these activities, there are multiple opportunities. One example is the Behavioral Risk
Factor Surveillance System (BRFSS) administered by the CDC, which includes two modules that states
can use to assess and track two issues critical to the health and well-being of older adults: the cognitive
decline module and the caregiver module. These two modules are currently voluntary and are in use in
35 states (21 caregiver and 21 cognitive decline, with seven states doing both modules). Public health
departments can advocate for wider implementation of these modules in states that have not adopted
these modules, and can analyze and disseminate the data in states that have.
Another example is the Survey of the Health of All the Population and Environment (SHAPE),
conducted in 2014 in six Minnesota counties. This study’s results have helped inform local priorities for
a number of populations, including older adults. For example, results on health and functioning were
included in a 2017 publication from Saint Paul – Ramsey County Public Health Department, Healthy
Aging: A Public Health Framework.
As another example, public health can provide important information about older adults using hotspot
analysis, a technique to examine the geographic distribution of populations, features, or events. Such
data can be essential in mapping neighborhoods in which older adults are at a higher risk for a fall or
have less access to a grocery store. This essential data can then be analyzed and disseminated to target
audiences in easy-to-use fact sheets.
Older adults often experience higher rates of injury and death and lower rates of economic recovery
following major natural disasters, such as earthquakes, floods, and tornadoes.
xl
Therefore, existing
datasets and hotspot analysis showing areas with high concentrations of older adults, particularly those
living alone or with a health challenge, could inform emergency preparedness. The Department of
Health and Human Services’ Office of the Assistant Secretary for Preparedness and Response developed
the emPOWER Initiative through a partnership with the Centers for Medicare and Medicaid Services.
The emPOWER Initiative provides federal data and mapping tools to local and state public health
departments to help them identify vulnerable populations who rely upon electricity-dependent medical
and assistive devices or certain health care services, such as dialysis machines, oxygen tanks, and home
health services. The emPOWER Map is a public and interactive map that provides monthly de-identified
Medicare data down to the zip code level, and an expanded set of near real-time hazard tracking
services. Together, this information provides enhanced situational awareness and actionable information
Page 10 | 18
for assisting areas and at-risk populations that may be impacted by severe weather, wild fires,
earthquakes, and other disasters. Public health and emergency management officials, AAAs, and
community planners can use emPOWER to better understand the types of resources that may be needed
in an emergency. For instance, these data can inform power restoration prioritization efforts, identify
optimal locations and needs for shelters, determine transportation needs, and anticipate potential
emergency medical assistance requests. The data are also used to conduct outreach prior to, during, or
after an incident, public health emergency, or disaster that may adversely impact at-risk populations.
The public health sector may also bring an asset-based approach to community assessment, documenting
the collective resources of older adults, their families, and their communities. This aligns with the work
of aging services and other providers to move away from an emphasis on deficits and toward a
recognition of strengths, skills, and capacities.
Public health can provide health care systems with critical info about older adults in their surrounding
communities as part of Community Health Needs Assessments, which are now mandated for all tax-
exempt hospitals by the ACA. Nonprofit hospitals are now required at least once every three years to
assess and prioritize the health needs of their geographic community, and then develop and implement
action steps to address those needs.
xli
At least one local, state, or regional public health department must
be involved in this process. Public health can thus call attention to the needs of older adults and ensure
programs and resources are dedicated to this population.
4. Conducting, communicating, and disseminating research findings and best practices to
support healthy aging.
Rigorous translational research can empower individuals to engage in healthy behaviors, support the
provision of effective clinical services, and create safe and healthy community environments. Public
health researchers, policymakers, and practitioners can play a key role in supporting healthy aging by
conducting, communicating, and disseminating research findings and best practices, particularly in terms
of prevention and population health.
For example, public health is already serving this function in the area of cognitive health.
Approximately 10%, or 3.6 million, of all Medicare beneficiaries over the age of 65 living in the
community had some form of dementia in 2011.
xlii
CDC’s Healthy Brain Initiative promotes a role for
public health in maintaining or improving cognitive functioning in later life. As part of this initiative,
CDC worked with the Alzheimer’s Association to develop a guide (first in 2007, then updated in
2013
xliii
) outlining action items for public health officials to promote cognitive health, address cognitive
impairment, and support dementia caregivers. A key component of this initiative is supporting applied
research and translating evidence into practice for providers and policymakers. Public health can also
assist with neurocognitive disorder public awareness campaigns around modifiable risk factors, signs of
disease progression, strategies for addressing changes in behavior, and community supports. Public
health can also support the development and implementation of evidence-based programs and evidence-
informed policies.
In addition, there is a large body of research concerning healthy aging, yet limited clearinghouses for
interested parties to find best practices or resources. Public health organizations may provide central
locations for information on healthy aging, including best practices, tool kits, and research. The ready
Page 11 | 18
availability of such a site can assist other sectors and professions in their efforts to address the needs of
older adults.
5. Complementing and supplementing existing supports and services, particularly in terms of
integrating clinical and population health approaches.
The fifth proposed role for public health is complementing and supplementing existing supports and
services, particularly in terms of integrating clinical and population health approaches. Existing public
health programs address a wide range of health issues, from infectious disease to chronic disease; from
education campaigns that reach the general public to targeted and focused home visits by educators;
from the enforcement of environmental regulations addressing long-term health risks, such as lack of
clean air and water, to the response to rare and catastrophic events. Furthermore, public health is focused
on the entire life course, providing programs and policies, such as maternal and child health, workplace
safety, and tobacco-free initiatives, that ultimately support healthy aging later in life. Each of these
current activities could be assessed to determine if it is adequately meeting the needs of older adults and,
when necessary, modified to better do so.
For example, aging services are beginning to recognize the value of Community Health Workers
(CHWs), a public health approach that has long been working with populations with limited access to
formal health and social services. CHWs are trusted members of a community and conduct outreach,
provide education, and serve as a liaison to formal systems of support. Preliminary research indicates the
promise of CHWs for reducing health care costs, supporting transitions back home from the hospital,
and connecting low-income senior housing residents to community services.
xliv
This may be a
particularly effective strategy to address health inequities.
Public health can also complement existing programs for informal caregivers providing assistance to
older adults with disabilities. Community-based support for caregivers are often fragmented from each
other and disconnected from the health and long-term care systems.
xlv
The National Family Caregiver
Support Program, created by the federal Older Americans Act Amendments of 2000, provides a range of
services, including counseling, case management, respite care, and training, particularly in terms of
adapting to the caregiver role and developing strategies for self-care. Public health can provide critical
education and training on performing the tasks needed to support older care recipients, such as safely
bathing or transferring from a bed to a chair, or addressing the behavioral changes associated with
dementia.
Barriers to Creating an Age-Friendly Public Health System
While there was a clear consensus at the convening about the value of an age-friendly public health
system, there was also a recognition that this expanded focus will be accompanied by barriers.
The first barrier is the need to break down professional and disciplinary silos. Promoting a public health
strategy to healthy aging requires a collective impact approach that recognizes that the solutions to
complex social problems do not emerge from the activities of a single individual, social service agency,
or sector, but rather from the activities of multiple entities, including businesses, nonprofits,
governments, and the general public.
xlvi
However, forming and maintaining collaborations of diverse
partners requires time, energy, dedication, and funding. Helping stakeholders who have not traditionally
Page 12 | 18
focused on older adults recognize the role that they can play to promote healthy aging across the life
course will be an additional challenge. As noted above, those in the public health sector are often
accustomed to convening and facilitating diverse collaborations and may be well suited to bring together
the wide range of stakeholders needed to promote healthy aging.
The second barrier relates to the persistence of ageist norms. In the United States, older adults are often
seen primarily as needy or helpless patients rather than as full human beings with strengths as well as
limitations, who can give as well as receive. Such limited perceptions foster the view of the aging of the
US population as a problem. At the same time, with a few notable exceptions, ageism also prevents the
needs of older adults from becoming a priority at the local, state, and federal levels. In an effort to
combat the deleterious effects of ageism, eight leading aging organizations (AARP, American
Federation for Aging Research, American Geriatrics Society, American Society on Aging,
Gerontological Society of America, Grantmakers in Aging, National Council on Aging, and National
Hispanic Council on Aging) have partnered for the Reframing Aging Project. By incorporating the
needs and assets of the aging population into its own priorities, public health can serve as a model for
other sectors and professions to embrace an aging-in-all-policies-and-practices approach. Through
assessment and research activities that complement the work of others, public health can highlight the
ways older adults are assets to their families and communities, and promote the message that the aging
of the population is a success story and not a crisis.
Finally, there is clearly a need for more funding from both the public and private sectors to support
healthy aging. Indeed, as the number of older adults continues to grow in this country, the amount of
public health and social service funding from the federal, state, and local levels is shrinking.
Furthermore, funding is rarely available for the larger scale, collective impact activities required to fully
support healthy aging. Grants are often given to one specific agency to support one specific intervention
for one specific health or social problem. Promoting healthy aging across diverse populations will likely
require a substantial investment of financial and human resources. However, stakeholders can develop
strategies to maximize existing resources and identify new sources of support. These include focusing
on relatively low-cost policies and programs, enlisting the participation of multiple stakeholders,
considering how existing policies and programs can meet the needs of older adults, and braiding
together funding from multiple sectors.
Next Steps
Despite these barriers, this is the time for public health to contribute to programs, policies, and
innovative interventions to promote health and well-being as people age. Given the changing
demographics and complex health-related needs of older adults, the public health sector should fully and
comprehensively make such work a priority. The Framework for an Age-Friendly Public Health System
highlights five key potential roles for public health. While this summary offers some examples of each, a
key next step is a more systematic approach to develop and disseminate case studies, best practices, and
tool kits.
Public health has a lot to offer – it has long utilized prevention and health promotion strategies that can
be usefully deployed. The Florida convening demonstrated that many aging service organizations are
eager to have partners from public health and other fields. Healthy aging depends on both upstream and
downstream efforts. Both efforts require the involvement of diverse sectors, disciplines, and professions
Page 13 | 18
and the consideration of the ways in which their policies, programs, and infrastructure affect older
adults. To ensure such policies are evidence-informed, aging and public health need to communicate,
collaborate, and leverage each other’s strengths and areas of expertise.
Page 14 | 18
Participant List
John Auerbach
President and CEO
Trust for America’s Health
Kathy Black
Professor
University of South Florida, Sarasota – Manatee
Alice Bonner
Secretary
Mass. Executive Office of Elder Affairs
alice.bonner@state.ma.us
Debra Burns
Director, Centers for Health Equity and
Community Health
Minnesota Department of Health
Terry Fulmer
President
The John A. Hartford Foundation
Trina Gonzalez
Program Officer
Milbank Memorial Fund
Chuck Henry
Administrator
Florida State Department of Health, Sarasota
Randall Hunt
President & CEO
Senior Resource Alliance
Kathryn Hyer
Professor
University of South Florida
Jeffrey Johnson
Director
AARP Florida State
Jennifer Johnson
Division Director, Public Health Statistics and
Performance Management
Florida Department of Health
Paul Katz
Professor & Chair, Department of Geriatrics
Florida State University
Aldiana Krizanovic
Senior Health Policy Consultant
Florida Blue Foundation
Jewel Mullen
Former Principal Deputy Assistant for Health
Health and Human Services
jmullen@livinglongerbetter.net
Celeste Philip
Surgeon General and Secretary of Health
Florida Department of Health
celeste.philip@flhealth.gov
Susan Ponder-Stansel
President
Florida Council on Aging
Richard Prudom
Deputy Secretary/Chief of Staff
Department of Elder Affairs
Sharon Ricks
Regional Health Administrator
U.S. Department of Health and Human Services
Page 15 | 18
Laurence Solberg
Chief, Division of Geriatrics
University of Florida
Nora Super
Chief, Programs and Services
National Association of Area Agencies on
Aging
Michele Walsh
Associate Director for Policy and
Communication
Division of Population Health,
U.S. Centers for Disease Control and Prevention
Staff and Consultants
Ashley Ashworth
Former Health Policy Analyst
Trust for America’s Health
Abby Dilley
Vice President of Program Development
RESOLVE
Sherry Kaiman
Strategic Partner
RESOLVE
LaToya Ray
Office Manager and Grants Manager
Trust for America’s Health
Partners
The John A. Hartford Foundation
The John A. Hartford Foundation, based in New York City, is a private, nonpartisan, national
philanthropy dedicated to improving the care of older adults. The leader in the field of aging and health,
the Foundation has three areas of emphasis: creating age-friendly health systems, supporting family
caregiving, and improving serious illness and end-of-life care.
Milbank Memorial Fund
The Milbank Memorial Fund is an endowed operating foundation that works to improve the health of
populations by connecting leaders and decision makers with the best available evidence and experience.
Founded in 1905, the Fund engages in nonpartisan analysis, collaboration, and communication on
significant issues in health policy.

Page 16 | 18
Endnotes
i
National Prevention, Health Promotion, and Public Health Council (2016). Healthy Aging in Action: Advancing
the National Prevention Strategy. Modified from Rowe, JW, Kahn, RL (1998). Successful Aging. New York:
Pantheon. And Marshal, VW, Altpeter, M (2005). Cultivating social work leadership in health promotion and aging:
Strategies for active aging interventions. Health & Social Work, 30, 135-144. Retrieved from:
https://www.surgeongeneral.gov/priorities/prevention/about/healthy-aging-in-action-final.pdf.
ii
Cutler, D, Miller, G (2005). The role of public health improvements in health advances: The twentieth-century
United States. Demography, 42(1), 1-22.
iii
Kane R. Public health paradigm. In: Hickey T, Speers MA, Prohaska TR, eds. Public Health and Aging.
Baltimore, MD: Johns Hopkins University Press; 1997:3–16.
iv
Anderson, L, Goodman, RA, Holtzman, D, Posner, S, Northridge, ME (2012). Aging in the United States:
Opportunities and Challenges for Public Health. American Journal of Public Health, Vol. 102, No. 3, p. 393.
v
Federal Interagency Forum on Aging-Related Statistics (2016). Older Americans 2016: Key indicators of well-
being. Washington, DC: Government Printing Office.
vi
Alzheimer’s Association. 2014 Alzheimer’s disease facts and figures. Retrieved from http://
www.alz.org/downloads/facts_figures_2014.pdf.
vii
Federal Interagency Forum on Aging-Related Statistics. Older Americans 2016: Key indicators of well-being.
Washington, DC: Government Printing Office.
viii
Federal Interagency Forum on Aging-Related Statistics. Older Americans 2016: Key indicators of well-being.
Washington, DC: Government Printing Office.
ix
Federal Interagency Forum on Aging-Related Statistics. Older Americans 2016: Key indicators of well-being.
Washington, DC: Government Printing Office.
x
Wallace, SP, Padilla-Frausto, D I, Smith, SE (2010). Older adults need twice the federal poverty level to make
ends meet in California (Policy Brief 2010-8). Los Angeles, CA: UCLA Center for Health Policy Research.
xi
National Health Policy Forum (2014). National spending for long-term services and supports, 2012. Retrieved
from: https://www.nhpf.org/library/the-basics/Basics_LTSS_03-27-14.pdf.
xii
Burman, LE, Johnson, RW (2007). A proposal to finance long-term care services through Medicare with an
income tax surcharge. Washington, DC: Urban Institute.
xiii
Komisar, HL, Feder, J, Kasper, JD (2005). Unmet long-term care needs: An analysis of
Medicare-Medicaid dual eligible. Inquiry, 42(2), 171-182.
xiv
Spillman, BC, Pezzin, LE (2000). Potential and active family caregivers: Changing networks and the “sandwich
generation.” Milbank Quarterly, 78(3), 347–374.
xv
Redfoot, D, Feinberg, L, Houser, A (2013). The aging of the baby boom and the growing
care gap: A look at future declines in the availability of family caregivers. Washington,
DC: AARP Public Policy Institute.
xvi
Rosenbloom, S, Herbel, S (2009). The safety and mobility patterns of older women: Do current
patterns foretell the future? Public Works Management & Policy, 13(4), 338–353.
xvii
West, LA, Cole, S, Goodkind, D, He, W (2014). 65+ in the United States: 2010. Retrieved from:
https://www.census.gov/content/dam/Census/library/publications/2014/demo/p23-212.pdf.
xviii
AARP Public Policy Institute and National Alliance for Caregiving (2015). Caregiving in the US. Retrieved
from: http://www.aarp.org/content/dam/aarp/ppi/2015/caregiving-in-the-united-states-2015-report-revised.pdf.
xix
US Census Bureau (2014). Coresident grandparents and their grandchildren: 2012. Retrieved from:
https://www.census.gov/content/dam/Census/library/publications/2014/demo/p20-576.pdf .
xx
World Health Organization (2007). Global age-friendly cities: A guide. Geneva, Switzerland:
World Health Organization.
xxi
Alley, D, Liebig, P, Pynoos, J, Banerjee, T, Choi, IH (2007). Creating elder-friendly communities: Preparations
for an aging society. Journal of Gerontological Social Work, 49(1-2), 1-18.
xxii
World Health Organization (2007). Global age-friendly cities: A guide. Geneva, Switzerland:
World H
ealth Organization.

Page 17 | 18
xxiii
Fulmer, T, & Berman, A (2016). Age-friendly health systems: How do we get there? Health Affairs Blog. DOI:
10.1377/hblog20161103.057335.
xxiv
Nelson, M.E, Rejeski, WJ, Blair, SN, Duncan, PW, Judge, JO, King, AC, ... & Castaneda-Sceppa, C, et al
(2007). Physical activity and public health in older adults: recommendation from the American College of Sports
Medicine and the American Heart Association. Circulation, 116(9), 1094.
xxv
US Department of Health and Human Services. HP2020 Objective Data Search website. Physical Activity.
http://www.healthypeople.gov/2020/data-search/Search-the-
Data?f%5B%5D=field_topic_area%3A3504&pop=&ci=&se=.
xxvi
Schutzer, KA, Graves, BS (2004). Barriers and motivations to exercise in older adults. Preventive
medicine, 39(5), 1056-1061.
xxvii
Clark, DO (1999). Identifying psychological, physiological, and environmental barriers and facilitators to
exercise among older low income adults. Journal of Clinical Geropsychology, 5(1), 51-62.
xxviii
Golden, J, Conroy, RM, Bruce, I, Denihan, A, Greene, E, Kirby, M, Lawlor, BA (2009). Loneliness, social
support networks, mood and wellbeing in community-dwelling elderly. International Journal of Geriatric
Psychiatry, 24(7), 694-700.
xxix
US Census Bureau. (2014). 65+ in the United States: 2010. (Publication P23-212). Washington, DC: U.S.
Government Printing Office.
xxx
Golden, J, Conroy, RM, Bruce, I, Denihan, A, Greene, E, Kirby, M, Lawlor, BA (2009). Loneliness, social
support networks, mood and wellbeing in community-dwelling elderly. International Journal of Geriatric
Psychiatry, 24(7), 694-700.
xxxi
Lauder, W, Sharkey, S, Mummery, K (2004). A community survey of loneliness. Journal of Advanced Nursing,
46(1), 88-94.
xxxii
Pinquart, M, Sorensen, S (2001). Influences on loneliness in older adults: A meta-analysis. Basic and Applied
Social Psychology, 23(4), 245-266.
xxxiii
Lyyra, T, Heikkinen, R (2006). Perceived social support and mortality in older people.
Journals of Gerontology: Series B: Psychological and Social Sciences, 61, S147-S152.
xxxiv
Bassuk, SS, Glass, TA, Berkman, LF (1999). Social disengagement and incident cognitive decline in
community-dwelling elderly persons. Annals of Internal Medicine, 131, 165–173.
xxxv
Village to Village Network (n.d.). Village map. Retrieved from:
http://www.vtvnetwork.org/content.aspx?page_id=1905&club_id=691012
xxxvi
Graham, CL, Scharlach, AE, Price Wolf, J (2014). The impact of the “Village” model on health, well-being,
service access, and social engagement of older adults. Health Education & Behavior, 41(1S), 91S-97S.
xxxvii
Healthy People 2020 (OA-1 and OA-2, respectively). http://www.healthypeople.gov/2020/topics-
objectives/topic/older-adults/objectives#4976.
xxxviii
Halloran, L (2013). Health promotion and disability prevention in older adults. Journal for Nurse
Practitioners, 9(8), 546–547. doi:10.1016/j.nurpra.2013.05.023.
xxxix
Shenson, D, Moore, RT, Benson, W, Anderson, LA (2015). Polling places, pharmacies, and public health:
Vote & Vax 2012.
xl
Bolin R, Klenow DJ. Response of the elderly to disaster: An age-stratified analysis. Intl J Aging and Human
Development 1982–3;16(4):283–297.
xli
US Centers for Disease Control and Prevention, Office for State, Local, and Territorial Support (2013). Summary
of the Internal Revenue Service’s April 5, 2013, notice of proposed rulemaking on community health needs
assessment for charitable hospitals. Retrieved from: http://www.astho.org/Summary-of-IRS-Proposed-Rulemaking-
on-CHNA/.
xlii
Federal Interagency Forum on Aging-Related Statistics. (2016). Older Americans 2016: Key indicators of well-
being. Washington, DC: Government Printing Office.
xliii
Alzheimer’s Association and US Centers for Disease Control and Prevention (2013). The Healthy Brain
Initiative: The Public Health Road Map for State and National Partnerships, 2013-2018. Chicago, IL: Alzheimer’s
Association. Retrieved from: https://www.cdc.gov/aging/healthybrain/roadmap.htm.
xliv
Rush, CH (2015). Community health workers moving to new roles as more seek to age in place. AgeBlog.
Retrieved from: http://www.asaging.org/blog/community-health-workers-moving-new-roles-more-seek-age-place.

Page 18 | 18
xlv
Riggs, JA (2003). A family caregiver policy agenda for the twenty-first century. Generations, 27(4), 68-73.
xlvi
Kania, J, Kramer, M (2011). Collective impact. Stanford Social Innovation Review, 9(1), 36–41.
